Leonardo Marini explains how using sequential, multilayer fractional and full beam Q-switched laser technology can improve tattoo removal results.
Tattoos and body piercings have become popular among young adults in most developed countries around the world, and this trend seems to be progressively increasing1. The reasons behind the tattoo phenomenon remains a mystery, even if most tattoo bearers confirm a ‘personal’ need for individuality and identity with specific groups2. However, progressive social interactions and specific working environments may induce tattoo bearers — women more than men — to seek medical assistance to remove their tattoos. Reasons and contributing factors for tattoo removal have been recently analysed, and include fear of negative comments and improving ‘self identity’3.
Additionally, numerous studies have confirmed that tattoo pigments do not remain in the dermis. With time, they are progressively transferred to regional lymph nodes through lymphatic vessels. Ink pigments within lymph nodes might affect medical interpretations during diagnostic and surgical procedures4-5. This side-effect is not widely known but public awareness campaigns will presumably contribute to decrease tattoo procedures as well as increase tattoo removal in the near future.

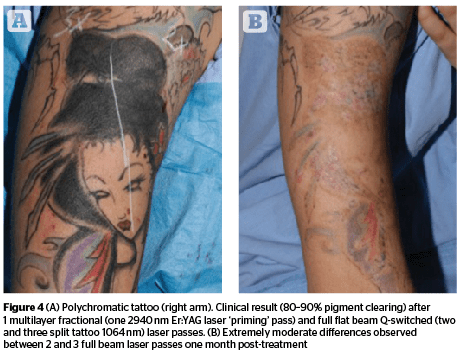
An interesting multilayer, full beam Q-S laser procedure (R-20) has recently been presented with the aim of reducing the total number of laser sessions10. Unfortunately, this innovative approach has been considered too complex to be routinely used in clinical practice, since 20 minute intervals between laser passes was considered excessively long. These intervals were necessary to eliminate sub-epidermal gas bubbles generated by the Q-S photo-acoustic effect, before proceeding with subsequent laser passes. Topical application of perfluorodecalin was reported useful in reducing inter-laser-pass intervals and the overall duration of the original R-20 procedure11. The author thought to ‘prime’ tattoos with a preliminary micro-ablative (2,940 nm Er:YAG or 10,600 nm CO2) fractional pass or micro-acoustic 1064 nm Q-S fractional pass before performing two or three full beam Q-S laser passes to eliminate gas bubbles through the many micro-holes created by the first pass12. The author was then able to reduce tattoo pigments by 80% after a single session and reach an almost complete pigment clearance in 4–6 sessions in the majority of tattoos treated with this technique. Picosecond laser systems claim to clear tattoo pigment faster and better than Q-S nanosecond lasers but so far, fractional multilayer Q-S procedures seem to produce quite similar results13–16.
Tattoo pigment characteristics
Professional tattoos are created by skilful tattoo artists and a variety of pigments contained in water-based tattoo inks are used to produce this popular form of body art. Presently, there are few commonly implemented rules regulating composition, distribution, storage, and practical use applied to tattoo colour formulations. In 2003 and 2008, the European Commission published specific guidelines on the chemical composition of tattoo inks17-18. These recommendations were variably implemented by different State members. Tattoo inks can be easily purchased from international manufacturers and, besides water, contain glycerine, ethanol, and sometimes preservatives. Colour particles are composed of organic and synthetic pigments and are different in size (Table 1). The smallest are the black particles and consist of carbon particles with a mean diameter ranging from 41 to 165 nm. Most of the black particles (99.94%) are less than 100 nm in size. White pigments are usually the largest and consist of TiO2. Their diameter usually ranges from 317 to 738 nm, but some inks may contain particles less than 100 nm in size. Green, blue (phthalocyanines), red and yellow (azo-pigments) particles are between black and white pigments in size19.
Carbon black has been classified by the International Agency for Research on Cancer as possibly carcinogenic for human beings — partly based on inhalation studies in rats22. Biological damage from carbon black and ultrafine TiO2 is supposedly linked to their inflammogenic properties, through induction of reactive oxygen species (ROS)23. TiO2 nanoparticle studies, carried out on their potential carcinogenicity, gave conflicting results, with some authors suggesting a possible genotoxicity in vivo, but with primary particle size of around 21 nm24. This particle dimension has not been found in tattoo inks so far. Azo-pigments tend to decompose into known carcinogens when exposed to light and laser irradiation25–26. Carcinogenicity studies have demonstrated a possible link with bladder cancer in humans27. In spite of all these potentially alarming findings, the safety profile of tattoo pigments seems to be very good.
Biological behaviour in the skin
Tattoo procedures are based on the meticulous intra-dermal micro-invasive introduction of pigments that will inevitably trigger a cascade of reactions aimed at eliminating and/or isolating them from the body. Once deposited in the dermis, colour micro-particles are progressively trapped into lysosomes within phagocytic dermal cells — mostly fibroblasts, macrophages, and mast cells.
Colour particle size seems to influence their local distribution within anatomical structures after their injection. Larger particles tend to remain in proximity of their initial deposition while NPs may reach the blood circulation and body organs, such as kidneys, liver, spleen, brain, and lungs. The liver and spleen are considered the main sites of NP accumulation29. In any case, once introduced in the dermis, tattoo pigments are there to stay within the body for a lifetime and can induce transient or persistent health problems related to their intrinsic chemical and physical characteristics, injection sites, and tattoo sizes30. Permanent tattoo pigment accumulation within regional lymph nodes can mimic intra-nodal calcium deposits during X-ray diagnostic procedures, making histologic examination necessary when non-benign etiologies are suspected31. Intra-operative observation of darkly pigmented tattoo-related lymph nodes could be interpreted as metastatic disease during sentinel lymph node procedures performed on melanoma patients32–36.
Laser specific interactions
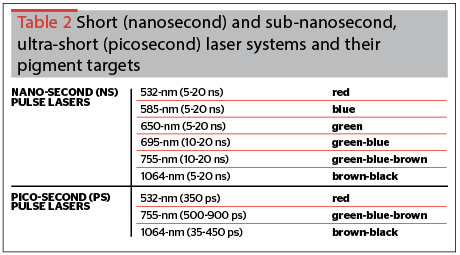
Among the procedures proposed to clear tattoos, short-nanosecond and ultra-short, picosecond laser systems are presently considered the gold standard to remove tattoo pigments37–38 (Table 2). The first non-scarring removal of black tattoo pigment was reported in 1983 by Reid et al., in Scotland using a Q-switched ruby laser39 (Figure 1).
A greater understanding of laser-tissue and tattoo pigment interactions have been made since, leading to the development of innovative technical and procedural improvements40. Traumatic tattoos and tattoos complicated by allergic-reactions have been successfully cleared by pigment-blind ablative fractional lasers41–42.
Like any light source, laser wavelengths used to remove tattoo pigments have different penetration depths. Shorter wavelengths penetrate less than longer wavelengths in biologic tissue. Short- and sub-nanosecond, ultra-short lasers are able to generate a specific photo-mediated light-chromophore interaction known as the ‘photo-acoustic effect’.
A photo-acoustic effect refers to any process where absorption of optical radiation leads to the generation of sound. It is produced when extremely intense (100 million W/cm2) laser pulses are delivered in an ultra-short amount of time (billionths of a second), producing extremely high temperatures (>300°C) within specific chromophores, such as tattoo ink particles. Only high peak power laser systems are able to generate a homogeneous top-hat energy distribution on relatively larger spots allowing for a deeper penetration.
This particular kind of absorption is able to generate an abrupt, extremely confined, photo-thermal effect within selected targets, along with intrinsic chemical and ultra-structural modifications related to extremely rapid volume changes. These effects are also associated with sudden mechanical waves generated by volume expansion to the surrounding tissue (thermo-mechanical effect)43.
Tattoo particles are fractured and undergo chemical and structural changes leading to modifications of their optical properties. Intracellular water within pigment-containing cells abruptly reach boiling temperatures leading to intracellular volumetric expansion, cell membrane explosion, and subsequent release of laser-modified tattoo particles into surrounding dermal structures. Once free again, part of the fractured tattoo pigments will be ‘absorbed’ by the local lymphatic system, part will be eliminated through trans-epidermal ‘extrusion’, and part will be slowly re-phagocytosed by dermal cells explaining the variable degree of pigment persistence after each laser treatment.
It is theoretically possible to recognize three aspects of laser-induced collateral photo-acoustic tissue interaction:
- The initiation of the acoustic wave — sudden thermal expansion due to rapid energy deposition at the tissue surface by optical absorption; followed by explosive vaporization exceeding enthalpy for the phase change of water to gas; and then plasma formation due to extremely strong, non-linear optical absorption at the tissue surface caused by high-intensity laser pulses
- The propagation of the acoustic wave
- The mechanisms of injury — stress caused by the extremely steep pressure gradient of acoustic waves, and cavitation bubbles44.
Computer simulations confirmed that tattoo ink particle break-up processes are photo-mechanically mediated. Minimal collateral tissue damage is generated when proper laser parameters are used. Laser pulse duration must be shorter than the thermal diffusion time across a characteristic length, linked to particle diameter, and less than the stress confinement time of target particles. Laser energy deposition must, therefore, be both thermally and stress confined in order to physically disrupt tattoo particles45. Disruptive efficiency seems to increase with decreasing laser pulse duration46.
In spite of all these extremely interesting light-chromophore interactions, the single pass Q-switched laser technique usually requires an average of 8–12 sessions, and sometimes more, to clear tattoos. Recently introduced picosecond laser systems seem to require an average of 4–6 sessions to obtain similar results.
Laser-assisted Q-switched and picosecond laser treatments are not without risks and side-effects. They are nevertheless minimal in comparison to millisecond laser and intense pulsed light systems, which should not be used to clear tattoos47–51 (Table 3).
Combined multilayer Q-switched laser procedures have been proposed to improve tattoo removal. In a study conducted by Kossida T et al., up to four subsequent laser passes were performed during the same treatment session (R-20 method). Twenty-minute inter-pass intervals were considered necessary to allow cavitation bubbles escaping through epidermal layers10. This innovative treatment, even if quite difficult to reproduce in clinical practice due to its complexity, was able to significantly reduce the number of sessions necessary to clear tattoos with minimal, transient side-effects. Topical application of perfluorodecalin has been proposed to clear post-QS laser epidermal whitening. A few seconds was reported to be sufficient in order to clear sub-epidermal cavitation bubbles, significantly decreasing the overall R-20 procedure treatment time11.
Tattoo removal with ablative fractional laser systems
Modern ablative laser technologies and pulse energy modulation have revolutionized operator control on photo-thermal vaporization of biological tissue using 2940 nm Er:YAG and 10,600 nm CO2 laser systems53–58. Recently, micro-ablative fractional technology was also successfully associated with Q-switched laser tattoo removal, opening new horizons in skin rejuvenation procedures59.
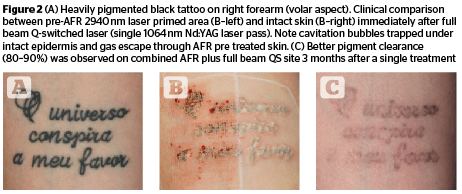
Ablative fractional laser technology (AFLT) has been successfully used in tattoo removal procedures, either alone or in combination with Q-switched laser systems. (Figure 2) Micro-surgical laser ablation of thin, vertical skin columns has proven effective in removing portions of tattoo pigments through direct destruction and external elimination of microscopic necrotic debris (MEND). 2940 nm Er:YAG and 10,600 nm CO2 ablative tattoo removal does not modify the chemical-physical structure of tattoo pigments since both systems operate within millisecond pulse ranges. Residual ink particles are partly re-phagocytised by dermal fibroblasts and partly drained by the local lymphatic system39–40. This particular laser approach will significantly decrease the overall quantity of potentially dangerous tattoo particles through trans-epidermal elimination.
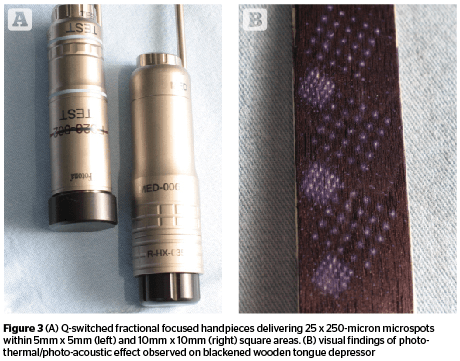
High energy fractional-mode 1064 nm Q-S laser systems can produce a relative colour-blinded, controlled tissue ablation through a combined mechanism of micro-thermal and photo-acoustic effects. This unique approach has the potential for generating a photo-mechanical disruption of ink particles, associated with a significant trans-epidermal elimination of pigments12 (Figure 3). Two of the three main points proposed to improve the efficiency of laser-assisted tattoo removal: increasing trans-epidermal elimination of ink particles, and optimizing lymphatic transport, will therefore be implemented52.
Ablative fractional laser technology (AFLT) has also been successfully used to improve the cosmetic and functional aspects of scars60–62.
Cosmetic tattoos can sometimes be associated with perceptible textural skin changes due to a variable degree of scarring produced by the mechanical perforations of dermal layers during the initial transfer of tattoo ink into the skin. These thin, irregular scar layers are responsible for increased light diffraction during laser treatments, negatively influencing the overall efficiency when using picosecond and Q-switched nanosecond non-ablative mode lasers. Lasers using ablative fractional technology (AFT) are not affected by dermal scarring when considering their overall efficiency in destroying tattoo pigments. They can also contribute to improve the textural quality of tattooed skin through progressive dermal remodeling41–42.
Innovative combined laser-assisted tattoo treatments
In an attempt to optimize tattoo removal procedures, new innovative laser strategies have recently been proposed with variable degrees of clinical success. As in many other fields of modern laser dermatology, sequential combinations of multiple laser passes have demonstrated better clinical results than single technologies used alone63–65. Focusing our attention on time-honoured Q-switched lasers, it has been demonstrated that multiple sequential passes, performed during the same tattoo removal session, were able to enormously enhance the efficiency of intra-dermal pigment clearing, without increasing complications and side-effects10. Sequentially combining 2940 nm Er:YAG or 10,600 nm CO2 ablative fractional resurfacing with full beam Q-switched lasers has proven more efficient than each laser technique used alone12,41,52,65.
Laser-assisted tattoo removal is not a painless procedure, particularly when larger anatomical areas and multiple passes are considered. Therefore, the author administered subdermal local anaesthesia to all treated tattoo sites (1% mepivacaine plus 1:200,000 epinephrine). Epinephrine was chosen to induce a temporary vasoconstriction able to reduce unnecessary light absorption by haemoglobin during the laser procedure. Besides laser proof goggles, a suitable form of ear protection is also required, since the Q-switched photoacoustic effect generates a high pitch noise during operation.
Wound healing
All treated sites followed a three-step dressing strategy aimed at providing a suitable environment to optimise wound healing. Immediately after each laser procedure, and during the full duration of the acute inflammatory healing phase, all treated tattoo sites were covered with sterile paraffin impregnated gauze and a thin layer of a hydro-active colloid alginate dressing formulation (Flaminal Forte, Flen-Pharma, Belgium), with excellent hygroscopic and anti-microbial properties. This specific medical device enhances trans-epidermal ‘extraction’ of tattoo micro-particles freed by laser procedures, while creating a hostile environment to microorganisms.
A final cover was provided by a sterile absorbing pad and TNT gauze. Class 1 compression stockings were prescribed for tattoos located on the lower extremities in order to help lymphatic drainage. Patients were instructed to remove their compression stocking at night.
Detailed written instructions were provided to standardize dressing procedures at home. The dressing sequence was performed 2–3 times per day, during the first 3–5 days post-treatment, or until trans-epidermal oozing stopped.
The second dressing stage, designed to assist the proliferating phase of wound healing, consisted of a topical application of sterile silicone gel (Stratamed, Switzerland) to provide a full contact, surface-conforming, semi-permeable transparent film, able to protect the newly formed epidermis from dehydration and potential micro-environmental irritations. Once dried, the thin silicone film was covered by a ultra-thin hydrocolloid pad to further protect treated areas by involuntary mechanical trauma. This dressing sequence was performed once a day until a uniform, perfectly flat pinkish epidermis was observed. Distally located tattoos on limbs required longer healing time and patients were preliminary informed.
The last dressing sequence was studied to optimise the early remodelling phase of wound healing and consisted of a topical application of a super-potent, class 1, steroid (0.05% clobetasol propionate) to be continued twice a day for 2–3 consecutive days per week — with the purpose of controlling excessive localized neo-angiogenesis. Pulsed steroid treatment continued for one/two months. A topical wound remodelling cream (i.e. Cicalfate-Avene, France, or Cicaplast baume B5-La Roche Posay, France) was prescribed to be liberally applied — a minimum of 2–3 times a day — during the same dressing phase and until the next laser session.
The author is very keen on the post-tattoo laser treatment dressing sequence since tattoo sites require multiple laser sessions to be cleared. Dermal-epidermal tissue needs to fully recover before planning subsequent laser treatments in order to tolerate repetitive micro-wounding and the subsequent inflammatory response. Up to 90% of treated tattoos (20 cases) demonstrated almost complete pigment clearing after 5 sessions.
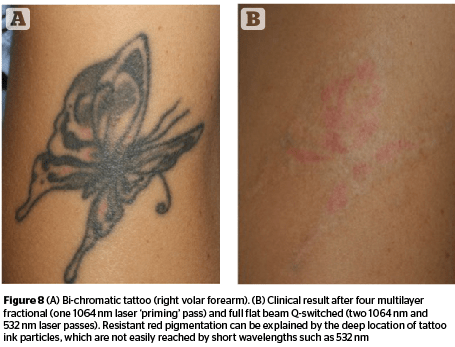
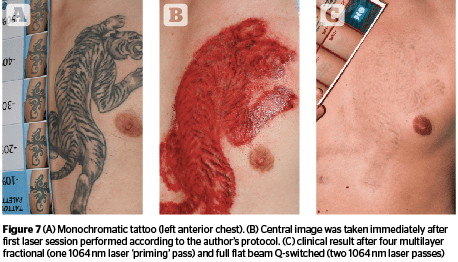
Preliminary ‘fractional priming’ was performed with a fractional Q-switched handpiece, able to generate twenty-five 250-μm micro-spots within an area of 5 mm x 5 mm. A 1,064 nm Nd:YAG wavelength was selected because of its deeper optical penetration. High energies, up to 12.7J/cm2, and stacking pulses, between 6–10, were used to completely cover all tattoo areas. Capillary bleeding was observed from each photo-acoustic micro-ablative spot, confirming the author was able to reach the papillary and upper reticular dermis (Figures 6–7). Five-minute intervals were sufficient to stop capillary bleeding, allowing the following full beam laser passes to be safely and efficiently performed. The same successful clearing rate was observed after the first laser sessions in the majority of tattoos (up to 80%). Up to 90% of treated tattoos (20 cases) showed an almost complete pigment clearing after 4 sessions (Figure 8). Interestingly, the author was able to improve both skin colour and textural irregularities of difficult-to-treat resistant tattoos, after up to 16 previously performed laser treatments.
Patient compliance and satisfaction levels were extremely high, due to the important pigment reduction observed after the first laser treatment, a painless procedure, and standardized dressing sequence.
Conclusions
Laser-assisted tattoo removal is gaining momentum in the complex scenario of modern dermatologic laser applications. The increasing number of tattoo bearers seeking medical advice to eliminate recent and old tattoos has prompted dermatologists and laser researchers to come up with new, innovative treatment strategies and techniques. Presently, time-honoured short-pulse Q-switched lasers seem to withstand the challenge posed by the new generation of picosecond laser systems when used as part of innovative sequential combinations. Much has been discovered about the potential hazards linked to chemical and ultra-structural characteristics of tattoo pigments, and more needs to be studied. Even if tattoo ink particles remain in the body for life, techniques able to eliminate them, even partially, through the skin could reduce their potential biological hazards. Combination treatments with conventional millisecond and recently introduced Q-switched fractional laser systems as well as short- (nanosecond) and ultra-short (picosecond) full beam laser systems seem to be a winning combination to rapidly and effectively clear intra-dermal tattoo pigments increasing both their external elimination and internal redistribution within the lymphatic system.






