ABSTRACT
Interventions: UltraPulse® ActiveFX™ CO2 laser (Lumenis Ltd., Yokneam, Israel) or Deka SmartXide DOT™ CO2 laser (DEKA S.r.l., Florence, Italy). All participants received regional anaesthetic of lignocaine 2% plus adrenaline, topical anaesthetic of AneStop® 5 mg statim and Valtrex (valacyclovir) 500mg twice daily for 8 days (i.e. herpectic prophylaxis mandatory for all patients). A post-procedural advice sheet was given to patients, and codeine with paracetemol as required.
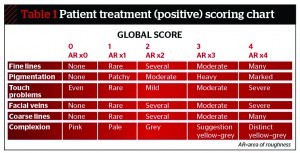
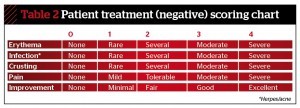
Main outcome measures: Participants’ global assessment of improvement (five-point Dover scale) at 2, 4 and 12 weeks. Reduction of rhytides, tactile roughness, pigmentation and blood vessels were recorded along with the re-ephithelialisation rate. The level of prolonged erythema and the presence of other side-effects such as infection were also recorded.
Results: Over 7 months, 23 subjects were randomised into a split-face study to compare the effects of two different fractionalised lasers on photoageing. Histological results initially showed that both lasers had a similar depth of penetration, but a greater thermal penetration effect was noted with the ActiveFx compared with the SmartXide, with consequential formation of increased neocollagenesis. Twenty-three patients (92%) in the ActiveFX group felt that their split face was completely better or improved compared with 21 (84%) in the SmartXide group (P<0.001). Fourteen patients (60.8%) said they preferred the SmartXide experience compared with nine patients (39.13%) in the ActiveFx group. One patient received full facial herpes. All patients received treatment to the neck.
Discussion: Although the two CO2 lasers initially appeared to produce equivalent clinical improvement of lesions and rythides, there was a marked difference noted at 3 months with the Lumenis ActiveFx showing superior new collagen formation.
Conclusions: The Lumenis ActiveFx gives a superior aesthetic outcome of the two lasers when examined at 3 months. It appears to have a deeper dermal penetrative effect, superior neocollagenesis, and is more suitable for the removal of more difficult lesions, such as large congenital nevi. The Deka SmartXide is an easy laser to use, but requires a separate plume extractor and re-do within a shorter period. Patients preferred the initial SmartXide effect.
Fractionalised laser skin resurfacing has become an important component of facial rejuvenation surgery as patients continue to seek less invasive procedures with a low downtime and low risk1. This change in attitude has also been prompted by a realisation of both doctors and patients that the much hyped non-ablative methods are not comparable with ablative skin resurfacing and were often subject to extravagant claims with regard to efficacy2–4. Until this time, CO2 laser resurfacing was considered the ‘gold standard’ for the treatment of rhytides and photodamaged facial skin5–10. Many practitioners went further and stated that the ultrapulsed CO2 laser was the most effective modality for repairing photodamaged skin as a result of years of exposure to harmful ultraviolet light11, 12. This photoageing effect is demonstrated clinically as a gradual deterioration of cutaneous structure and function. It manifests in the epidermis and upper papillary dermis by giving skin a roughened surface texture, as well as laxity, telangiectasia, wrinkles and varying degrees of pigmentation13, 14.
Although, ultrapulsed CO2 laser skin resurfacing was largely considered the best option for treatment of this type of photoaged facial skin, it also had certain post-procedural problems15–17. These included prolonged postoperative recovery, pigmentary changes and a high incidence of adverse side-effects, including acne flares and herpes simplex virus (HSV) infection18–20. Many patients also complained of oedema, burning, and erythema that sometimes lasted for a number of months21, 22. The delayed healing, implied risks and long downtime also made many patients reluctant to accept this method of treatment23, 24.
Fractional CO2 lasers
While non-sequential fractionalised technology is relatively new, its benefits of faster recovery time, more precise control of ablation depth, and reduced risk of post-procedural problems are already clear1. These lasers also reduce the consistently high levels of non-responders often seen with quite expensive non-ablative treatments that require many painful sessions25. The obvious benefits of these lasers have led to many new fractional resurfacing devices entering the market at the same time26.
The adoption of the newer fractionalised CO2 lasers by many physicians also appears to have reduced the morbidity associated with this type of treatment1. Damage to the epithelium is less apparent because unlike conventional ablation, some of the stratum corneum remains intact during treatment and acts as a natural bandage. This allows the skin to heal faster than if the whole area was treated, as the surrounding ‘healthy’, untreated tissue helps to fill damaged areas with new cells. Downtime is also reduced and erythema moderate, allowing patients to apply cosmetics 5 days after treatment27.
Fractionalised C02 lasers are extremely versatile as they can be used for the treatment of facial rhytides, acne scars, surgical scars, melasma, and photodamaged skin. There are currently a number of high-energy, fractionalised CO2 lasers available for cutaneous resurfacing. Although each laser system adheres to the same basic principles, there are significant differences with regard to tissue dwell time, energy output, and laser beam profile. These differences may result in variable clinical and histological tissue effects. The purpose of this study was to compare the in vivo clinical and histopathologic effects of two fractionalised CO2 resurfacing lasers: the 30 W SmartXide DOT™ (DEKA S.r.l., Florence, Italy) and the UltraPulse® ActiveFx™ (Lumenis Ltd., Yokneam, Israel). The ActiveFx (although technically the name of a set of parameters) is an upgrade of the UltraPulse Encore with a smaller spot size and a new computer pattern generator (CPG), giving a random pattern and thus reducing the possibility of adjacent spots with resultant heat accumulation. The SmartXide DOT adopts a lightweight titanium articulated arm in conjunction with a user-friendly colour touch screen control panel to display the settings. The SmartXide DOT requires an external plume device.
Patients and methods
A prospective randomised split-face study using two different fractionalised CO2 resurfacing lasers (Lumenis ActiveFX and Deka SmartXide) was performed on 23 Caucasian subjects (17 women) with visible evidence of cutaneous photoageing to compare the clinical efficacy of each device. All subjects were given a physical examination and their medical histories reviewed. Subjects were instructed to avoid sun exposure and apply SPF 50 daily for 1 week after the study period. The study evaluated post-procedural aesthetic results, length of downtime, adverse side-effects, and new collagen formation for the ActiveFX and SmartXide during ablative treatment for photodamaged facial skin.
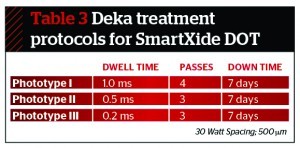
Each patient was randomly assigned to receive treatment on one half of their face with one of the devices. The ActiveFx patients were treated at an energy of 100–125 mJ, rate 125 Hz, CPG 3/6/1-3/9/4, repeat delay 0.5 s, depending on the area of the face being treated. This is approximately 19 W. This was dropped to 14 W for the neck area owing to the possibility of poor healing as a result of reduced epidermal rete pegs that project into the underlying connective tissue in this area compared to the face (rate 125 Hz, CPG 3/6/1-2, repeat delay 0.5–1 s; SmartXide at 10–15 W, 500 µm pitch, 500 ms dwell time). The SmartXide DOT patients were treated at a power of 30 W, Dot mode on, spacing 300–500 μm, dwell time 800–2000 μs, stack of 2 or 3. These levels were relatively arbitrary and not based on specific conversion tables, but the author was hoping to achieve an ablation depth of approximately 80 mm and a depth of the residual thermal damage of 200 mm28–30.
All patients underwent an ‘active’ single-session, single-pass and full-face fractional ablative treatment. Fifteen patients received a double-pass treatment of the periorbital region and 12 to the perioral area, and in these cases the effect was repeated bilaterally. Significant differences (P<0.05) between baseline and at 1 and 3 months post-treatment were observed for fine lines and wrinkles, although the best improvements were noted at regions in which the practitioner thought the patient required a double-pass. Patients who received second overlapping passes in the periorbital and perioral areas received them for deeper rhytides. The author went slightly above the recognised Lumenis ‘soft’ protocol for ActiveFx — energy 90–100 mJ, rate 100 Hz, CPG 3/5/2-3/5/5, repeat delay 0.5s — as previous experience showed these parameters to be less preferable in aesthetic effect. The protocols for the SmartXide included treatments that required multiple passes, so the above parameters were agreed with the company to be comparatively similar.