Chedly Bouzouaya combines a mini-incision with radiofrequency in his new technique to improve results
in lower eyelid blepharoplasty.
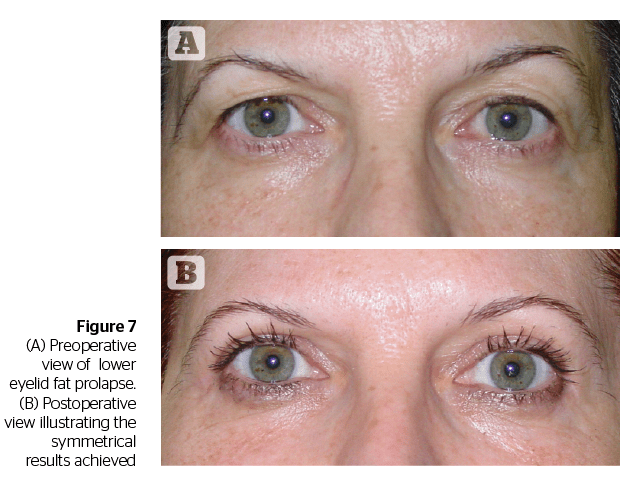
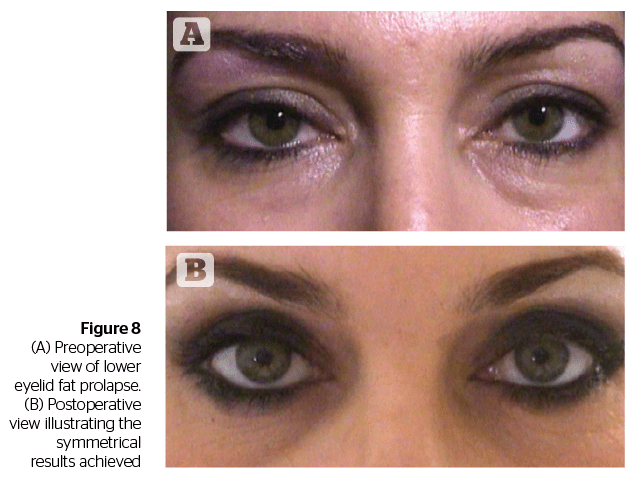
Lower eyelid blepharoplasty can be addressed with fat removal, fat repositioning, arcus marginalis release, and septal tightening. Whatever the approach, it is paramount to not alter the shape and contour of the eyelid fissure, to avoid any potential complication, and to allow a fast recovery for the patient. In this article, the author focuses on performing lower eyelid blepharoplasty on patients requiring a conservative herniated fat removal.
The transconjunctival approach to lower eyelid blepharoplasty has increased in popularity over the past few years. This is partly due to a greater awareness among patients of the potential complications of the transcutaneous approach, more people being interested in having a blepharoplasty, and because patients nowadays request blepharoplasty at an earlier age.
The author’s preference is to use radio-surgical instrumentation, which is the use of ultra-high frequency radio signals to incise, excise, ablate or coagulate tissue with minimal tissue alteration. Soft tissue resistance to these radiowaves causes the water cells to heat resulting in cellular molecular dissolution. The radiowaves leave the radiofrequency unit through a hand piece. A fine wire electrode attached to the handpiece is used to make a skin and muscle incision and is also used for orbital fat resection. The incision is pressureless, smooth, and bloodless with minimal to no lateral heat spread. High frequency waves in surgical procedures have been investigated for decades6 showing that 4.0 Mhz is the optimal frequency for cutting soft tissue and that a fully filtered wave produces minimal tissue alteration. The radiofrequency unit has the capacity to deliver a variety of waveforms:
- Fully filtered mode: 90% cutting and 10% coagulation for microsmooth cutting with little tissue damage and concomitant coagulation
- Cutting-coagulation mode: this waveform consists of 50% cutting and 50% coagulation. It is designed for equal amounts of cutting and coagulation, especially useful in vascular areas such as eyelids while maintaining minimal amounts of lateral heat and tissue damage
- Hemostasis mode: this waveform consists of 10% cutting and 90% coagulation and is designed for direct and indirect hemostasis techniques.
In comparison with the CO2 laser, radiosurgery causes less heat damage. Clinically, tissue incised using ultra‑high frequency radiosurgery at appropriate parameters, has no visible thermal artefacts and no predisposition toward wound dehiscence as seen post CO2 laser. Histopathologically, the cellular architecture disruption is less in tissue incised with a dual radiofrequency unit than with CO2 laser8–10.
Once you have the right instrumentation, the right technique will enhance your results, avoid complications, and allow your patient a rapid return to work and to normal social life.
Historically, the transcutaneous approach has been the surgical technique of choice to resect herniated fat, sometimes resulting in lower eyelid ectropion, noticeable scars, and lower eyelid retraction. The latter being the most common and dreaded complication of the transcutaneous lower eyelid blepharoplasty. The other complications are:
Excessive skin removal
- Rounded, blunted lateral canthus
- Excessive or insufficient fat removal resulting in over or under correction, diplopia or hemorrhage11,12.
The transconjunctival technique was first described in 1924 by Bourquet13. This approach was popularised by Tessier in 197314, who used the conjunctival approach to the orbital floor and maxilla in congenital malformation and trauma. The traditional conjunctival approach with incision extending from the punctum to the lateral canthus, can result in complications such as — although rare — cicatricial ectropion, lower eyelid retraction, canthal dehiscence, canalicular laceration, punctal eversion, excessive or insufficient fat removal, diplopia, hemorrhage, button hole laceration of the lower-eyelid, and conjuntival prolapse or chemosis. In this era of endoscopic surgery, mini-incision cataract surgery and phacoemulsification, suture techniques for facial rejuvenation and beautification, the mini-incision transconjunctival lower eyelid blepharoplasty achieves very good aesthetic results, but significantly reduces surgical manipulation and potential complications. It also allows for a faster recovery.
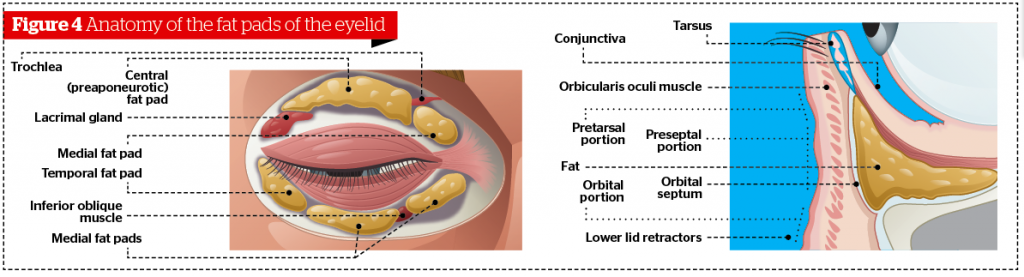
Anatomy
The lower eyelid is divided into an anterior lamella with skin and orbicularis and a posterior lamella with tarsus and conjunctiva. The capsulopalpebral fascia in the lower eyelid is analogous to the levator aponeurosis of the upper eyelid. It originates from attachments to the muscle fibers of the inferior rectus muscle. It divides as it encircles the inferior oblique muscle then joins to form Lockwood’s suspensory ligament. The capsulopalpebral fascia inserts onto the inferior tarsal border and sends strands to the inferior conjunctival fornix, the suspensory ligament of the fornix. The orbital septum, a multi-layered thin sheet of fibrous tissue, raises from the periosteum over the inferior orbital rim. The orbital septum fuses with the capsulopalpebral fascia at or below the inferior tarsal border.
There are three fat pockets in the lower eyelid: the medial, the central, and the lateral fat pocket. In transconjunctival blepharoplasty the entrance into the orbital fat is made posterior to the orbital septum. Therefore, the anterior lamella is not violated.
Surgical technique
The instrument used for this technique is the Ellman Surgitron (Hicksville, NY). This radiofrequency surgical unit delivers high frequency waves at 4.0 MHz, the optimal frequency to cut soft tissue. The Surgitron has the capacity to deliver a variety of waveforms. The one used for lower eyelid blepharoplasty is the cutting and coagulation mode, which is 50% cutting and 50% hemostasis15. The A3 electrode for the transconjuntival approach is used. Also, the new alloy micro-radio frequency electrodes require less power resulting in significant reduction in thermal temperature and tissue drag.
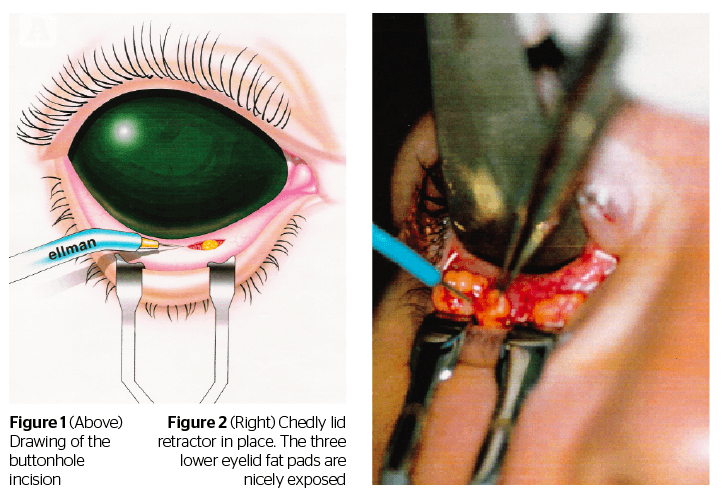
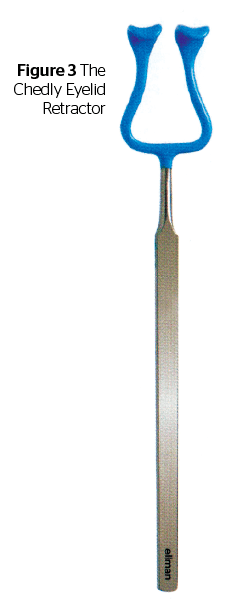
The anaesthesia is performed by infiltration of the fornix with 2–3 ml of 2% lidocaine with 1/100.000 epinephrine. An eyelid plate is placed achieving protection to the globe and helping the orbital fat to herniate. The fornix is exposed using the Chedly eyelid retractor, a specifically designed insulated retractor16, safe to use with the radiosurgical unit or CO2 laser. This retractor also facilitates the assessment of fat to be resected and allows the physician to cauterize any occurring bleeding easily.
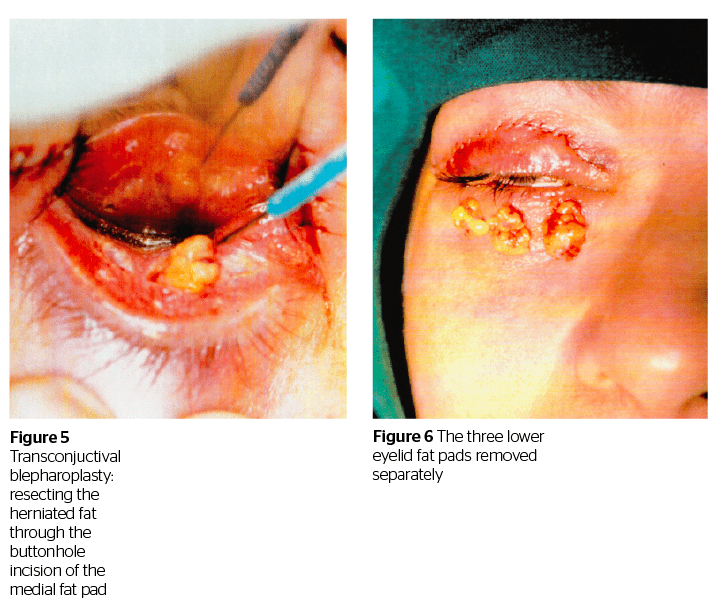
With the electrode attached to the handpiece of the radiofrequency unit, quick, light, smooth strokes are used to make a fine exact incision without charring, with minimal lateral heat spread or collateral tissue damage. An incision through conjunctiva and retractors is made at the lower border of the tarsal plate for the medial, the central, and the lateral fat pad (if a lateral fat prolapse has been assessed preoperatively).
With the eyelid plate pressure applied on the globe, the fat pad is teased out, held with forceps and resected using the radiosurgical unit. The fat is easily resected and if there is any bleeding, it is easily controlled by simply grasping the bleeding tissue with the forceps and touching it with the electrode. There is no need to change instruments or to clamp the fat with a hemostat across its base before resecting it and cauterizing the fat stump as is done traditionally. The amount of fat to be removed in each of the three fat pockets needs to be assessed preoperatively. With the mini-incision technique it is easier to accurately assess the amount of fat to be removed as the herniated fat ‘pops’ out through each of the three button hole incisions. In addition to this the fat is resected away from the deep structures such as the inferior oblique muscle. There is no need for sutures. A combination of antibiotic-steroids is placed in the fornix and ice packs are placed on the closed eyes.
Discussion


Conclusion
In cosmetic eyelid surgery there is a no tolerance for error and complications. The mini-incision for lower eyelid blepharoplasty is about minimal manipulation, minimal trauma, and minimal recovery time.
Patient selection, a thorough evaluation of the deformity and an accurate surgical procedure with the proper instrumentation remain key to obtaining optimal results.


 Excessive skin removal
Excessive skin removal