Daniel Chang covers the risks involved when using injectable products and outlines his key prevention tips, recommendations to help treat problems as they arise, and how to improve results in the future
Facial injections with either dermal fillers or botulinum toxin are some of the most popular aesthetic treatments currently available and their safety profile is extremely good. However, complications can and do occur and it is important the practitioner knows how best to deal with the situation they are faced with.
Doctor factors include technique and dilution. Good lighting and the use of magnifications loupes can help the practitioner perform the procedure more effectively and safely.
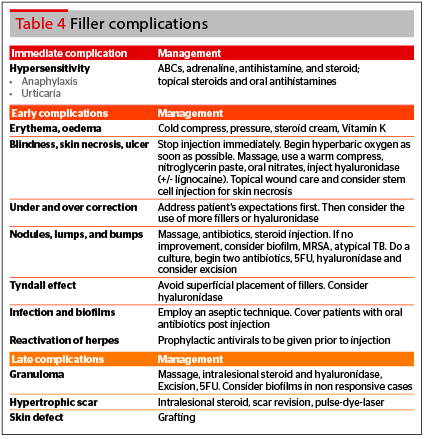
Product factors refer to the choice of botulinum toxin or filler used. Toxins have no long term sequelae, so management would refer to immediate and short-term measures only. Management can be divided into prevention and treatment. Table 1 divides botulinum toxin complications into common, serious, and self-limiting1,2.
Botulinum toxin complications
Common complications
These can occur in all cases, irrespective of the above factors, and include the following: redness, swelling, bruising, pain, and headache. These can be managed accordingly.
Pain can be reduced with emla cream, ice, pinching the skin, a slow injection speed, use of a smaller gauge needle, and preserved normal saline. Bruising can be reduced with arnica montana pre-injection, avoiding NSAIDS, good lighting and technique, stretching the skin before injection to visualise the blood vessels, and finger pressure3–6. Bruising can be treated with arnica, and headache can be improved with analgesia if needed.
Serious complications
These tend to be due to patient factors, and are commonly linked to a pre-existing condition. Hypersensitivity reactions, namely urticaria and anaphylaxis, are commonly caused by the components in botulinum toxin — primarily human albumin, lactose, and sodium succinate.
It is key to take a good history and identify any prior allergic reactions to botulinum toxin. These patients should not undergo toxin injections.
The focus for the treatment of serious complications is immediate action, identify anaphylaxis, and implement emergency measures. Ensure the airway is stable, breathing is adequate, and circulation intact. Delivery of supplemental oxygen and intravenous fluids is also important. Definitive treatment is the use of adrenaline, combined with antihistamines and steroids as adjuncts.
Self-limiting complications
These include erroneous muscle involvement, infection, and over or undercorrection. These are usually due to doctor factors, namely technique and dilution; as well as product factors, specifically the choice of botulinum toxin used7,8.
Muscle involvement in other groups can potentially be due to the product choice, namely Dysport (Ipsen Biopharmaceuticals, Inc, Basking Ridge, NJ) and Botox (Allergan, Irvine, CA). Studies have shown that Dysport has a wider diffusion radius than Botox, and can potentially affect other muscle groups9.
In prevention, the key is to respect facial anatomy, and inject in the correct area, with the correct dose. In terms of treatment for these complications, there is no quick fix. Patients need to understand that the effects are temporary.
Upper face complications include ‘Spock’ look, eyelid ptosis, brow ptosis, diplopia, and muscle asymmetry.
Brow ptosis can occur through in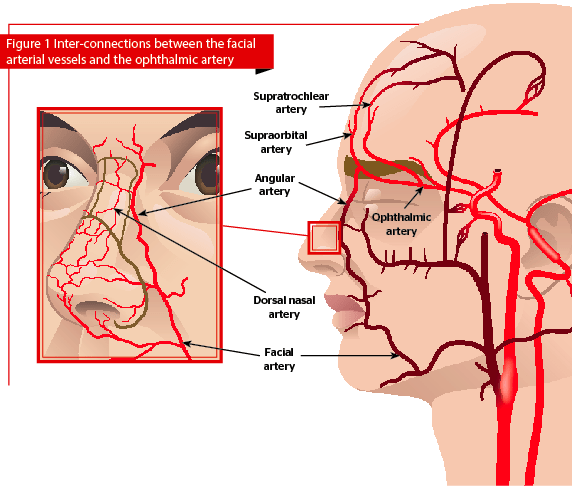
Eyelid ptosis can occur with crow’s feet and glabellar injections. To reduce this, avoid in older patients, and avoid injecting within 1 cm of the orbital rim. To correct, apply iopidine, 1 to 2 drops, three times a day. This can help with a 1 to 2 mm elevation.
The ‘Spock’ look can occur as a result of forehead injections. To correct this, inject 2 units in the lateral frontalis, 2 cm above the brow. Diplopia, ectropion, and asymmetric smile can occur after crow’s feet injections. This can be corrected by injecting 1 cm outside the orbital rim, and staying above the upper border of the zygoma. If diplopia occurs, you may cover the eye with a patch.
Midface complications include smile asymmetry, and perioral droop. Smile asymmetry can occur with masseter botulinum toxin injections. Injections should be placed deeply to avoid the risorius muscle and reduce risk of smile assymetry. Perioral droop can occur with injection to the depressor anguli oris muscle. To reduce perioral droop, make sure injections point laterally, while pinching the muscle in between your fingers.
Lower face and neck complications include dysphagia. The key is to pinch the platysma muscle between your fingers and inject a small dose superficially.
Infection
Treatments need to be performed in aseptic conditions. However, if infection occurs a short course of antibiotics, oral and topical, would be an option.
Over, under and no correction
Overcorrection leading to a ‘frozen’ look can occur when too much product is used, so it is good to start with a low volume and go slow. When overcorrection does occur, there is no quick fix. Reassure the patient that the effects are temporary. Undercorrection can happen too, and the solution is to inject a subsequent dose of toxin. No correction can occur with patients who develop immunoresistance to the toxin, or with patients who have static wrinkles. Poor injection technique and use of denatured toxin also contribute to the problem.
Special techniques and complications
A Botox lift is essentially upper, mid, and lower face intramuscular injections of conventional Botox, with the addition of platysma and depressor anguli oris injections, hence restoring the imbalance between levators and depressors of the face, and sharpening the contours. Side-effects occur from improper placement of toxins. Prevention of these side-effects includes having a good understanding of facial anatomy.
Dermalift is a botulinum toxin in diluted form, used to induce a skin tightening effect via intradermal injections. Side-effects occur from improper placement of the toxin, hence it is essential to stay intradermal. When under the skin, moving the needle downwards will cause dimpling. This means you are at the intradermal level.
Dermal fillers
Complications
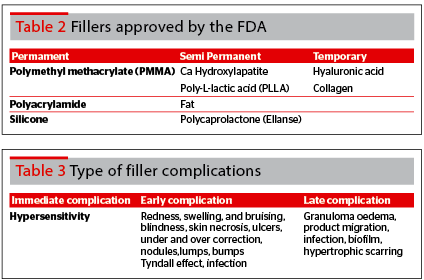
In general, permanent fillers are usually associated with adverse events. Problems tend to appear 5 to 7 years later, as a result of the immune response to the filler. It is understood that the immune system forms a capsule over the filler, and as the capsule tightens, a foreign body response or localised infection occurs. For example, permanent lip fillers can lead to intraoral lumps, which may hinder chewing. Tear trough permanent fillers may lead to fibrosis, and ectropion12.
In order to manage such complications, surgical excision or incision and drainage of the capsule is required in order to aspirate the contents. Following which, adjuncts would include antibiotics, hyperbaric oxygen, and use of plasma rich platelets to promote healing13–15.
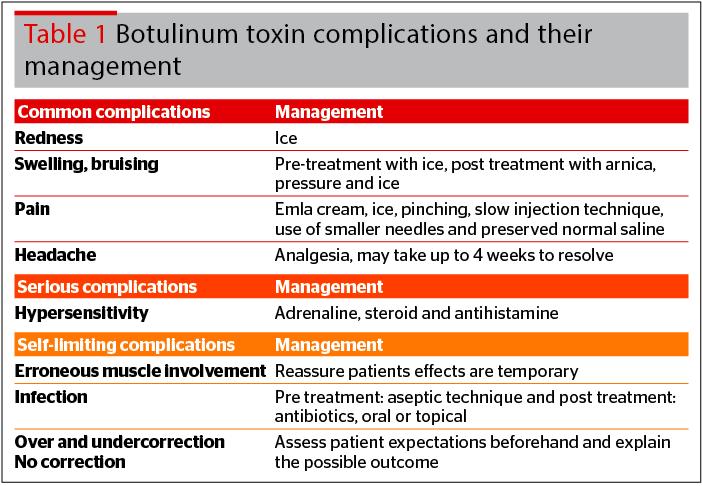
Filler complications may be classified into immediate, short term, and long term. They are related to type of filler material (product), patient selection, and injection technique. Common complications are redness, swelling, and bruising. Intravascular complications with fillers will be discussed in greater depth and detail further below.
Immediate complication
The key to dealing with hypersensitivity reactions, such as anaphylaxis, is to implement emergency measures immediately. Ensure the airway is stable, breathing is adequate, and circulation intact. Delivery of supplemental oxygen and intravenous fluids is also important. Definitive treatment is the use of adrenaline, combined with antihistamines and intravenous steroids as adjuncts.
Early complication
Addressing the undercorrection and overcorrection of fillers requires addressing patient’s expectations pre-treatment and showing them what can and cannot be achieved, and not selecting patients who have unrealistic expectations.
Lumps, nodules, and bumps can be managed with hyaluronidase injection, massage, aspiration, and in persistent cases, incision and drainage. The Tyndall effect can be prevented by not injecting too superficially. Management entails the use of hyaluronidase or making an incision in the skin and expressing the filler.
Infection and biofilms can be reduced with an aseptic technique pre-treatment, and the use of oral antibiotics post treatment16–19.
Vascular occlusion leading to blindness and skin necrosis will be discussed further below.
Long term (delayed) complications
Granuloma formation can be managed with intralesional steroids, antibiotics, and excision. Intravascular complications such as blindness, can occur as a result of injections in the glabellar area and the nose20–21.
 Anatomy
Anatomy
To understand the reason why blindness can occur, we need to take a look at the anatomy of facial blood vessels. Figure 1 is a drawing that illustrates the inter-connections between the facial arterial vessels and the ophthalmic artery.
During filler injections to the forehead and glabellar region, the injector must be mindful of the supratrochlear artery. This arises from the ophthalmic artery. In some cases, the supraorbital artery may be involved.
In filler treatments close to the nose, the injector needs to pay attention to the dorsal nasal artery, which also arises from the ophthalmic artery. Here, technique is important, and one needs to use a cannula, stay midline, and aspirate before using a retrograde injection in a slow and steady manner.
In fillers for the nasolabial folds, tear trough, anterior medial cheek and nose, one must be careful of the facial artery. The facial artery is a branch of the external carotid artery supplying the face, and ends as the angular artery at the medial canthus.
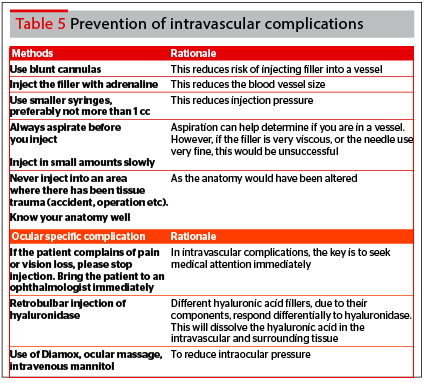
Prevention of intravascular complications
- Methods to reduce the risk of intravascular complications22–25:
- Aspirate before injection. If blood appears, the needle should be removed and injected at a different site
- Injections should be performed lightly and slowly, while moving the needle tip slightly
- Each bolus injection should be limited to 0.1ml thereby limiting the risk of a column of filler extending upstream
- Small syringes are preferred as the injector can better control the speed and volume injected
- Microcannulas reduce the number of entry points for filler injections, hence reducing the risk of intravascular compromise
- Consider adrenaline to promote vasoconstriction, reducing the size of vessels and risk of intravascular injection
- Avoid injection in areas with tissue trauma (accidents, surgery, etc).
Retrobular injection technique
- Evidence from cadaver dissections show near immediate elimination of the intravascular hyaluronic acid after hyaluronidase is injected next to the blood vessel using the retrobular injection technique:
- Local anesthetic is injected over the inferotemporal orbit at the lower eyelid
- Into the inferotemporal side of the orbit, a blunt cannula (25G), is carefully inserted, and should remain infraconal and inferolateral to the optic nerve
- In the inferolateral orbit, hyaluronidase is used.
- Finally, for early complications, the author will discuss infection and biofilms.
Infection and biofilms
Aetiology
Diagnosis
To diagnose, imaging with CT scan, MRI or PET can help to localise the foci of infection. Diagnosis is definitive through a biopsy.
Prevention and treatment
Benzalkonium chloride wash, having superior antiseptic strength compared to alcohol, should be used before injection. In persistent cases, after initial antibiotic and hyaluronidase treatment, one can consider using intralesional fluorouracil (5FU) injections every 4 weeks.

Management
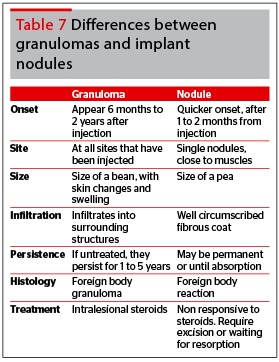
Intralesional steroids are effective for granulomas. The key is to identify early implant nodules, which form 2–4 weeks after injection, compared with foreign body granulomas, which appear after an incubation period of several months. Because foreign body granulomas are infiltrative in nature, surgical excision would not be the first choice.
In persistent cases, consider biofilms, such as atypical TB or MRSA. Do a culture and TB test. Start dual antibiotic therapy, 5FU, hyaluronidase, and consider excision.
Conclusion, critical analysis and future studies
Combination treatment is the gold standard
The current trend is moving towards the use of combination therapy to enhance skin rejuvenation. Combination therapy can potentially raise the bar for achievable results. On the flipside, we could see a rise in complication rates. This risk is further increased as more brands of fillers are introduced to the market, and the greater public awareness and acceptance of injectables.
Furthermore, new treatment paradigms, such as having an initial full treatment and subsequent top-ups to optimize results, will further drive the injectables market. This can be seen with the Galderma range of Skinboosters and Restylane fillers for nasolabial folds. Here are some proven combination therapies:
- Microbotox together with fillers for mild skin sagging
- Ultrasound coupled with the use of fillers and microbotox for skin lifting and tightening for moderate skin sagging. These work on different layers of the skin, from the SMAS layer through ultrasound energy, to the subcutaneous layer by fillers, and the intradermal layer with microbotox
- Threadlifts and ultrasound combined with fillers and microbotox for enhanced skin lifting and tightening. Threadlifts work to provide an anchor for the soft tissue. Maintenance with long pulse lasers in a vectoring direction can help to improve the durability of the result.
As such, further research would be needed to identify the types of combination, the sequence, timing, and number of sessions. Longer follow-up time and larger sample size clinical studies would help answer these questions.
The risk of semi permanent and permanent fillers
Skin healing, recovery, and anti-ageing
With more intensive treatments comes the need for healing measures to reduce downtime. As we know, the majority of skin rejuvenation techniques involve tissue injury to induce collagen stimulation. Hence, another avenue of research is treatments that can complement and aid in skin healing and recovery. Skinboosters, platelet rich plasma (PRP), and stem cells may provide the answer, and be a useful complement to the majority of skin rejuvenation procedures.
Skinboosters, through the microneedling technique and use of hyaluronic acid, help to boost skin hydration, healing, and recovery. These microneedles support the intradermal injection and deposition of the skinboosters into the dermis. The physical nature of the needle helps breach the epidermal barrier. Ongoing research is aimed at how to schedule skin rejuvenation techniques with this skin healing modality and what goes into the skinboosters26-27.
Touching on what goes into skinboosters, worldwide, Restylane has trademarked the name Skinboosters, which consisted of Restylane Vital and Vital light, both hyaluronic acids. Interestingly, Plastic Surgeon Dr Steven Liew has developed a mixture of 1 ml of uncross-linked hyaluronic acid filler with 10 units of botulinum toxin to re-create this skin hydration effect. He believes in the use of a machine to support multiple intradermal injections, hence ensuring consistency of technique28.
Let’s not forget about the use of PRP in skin healing. PRP contains different growth factors and cytokines to boost wound healing. This is yet another modality worth exploring to improve skin rejuvenation. A Korean study has found that topically applied PRP can help with fibroblast proliferation and collagen production to boost skin elasticity and healing. Hence, there is a role for PRP in filler related vascular complications like skin necrosis, and scarring29–30.
Presently, there is no standardized way to deliver PRP into the skin. More research in delivery with the use of microneedles need to be carried out to validate its efficacy in the arena of anti-ageing medicine.
Another arena worth looking into is adipose derived stem cells. With its multi-potency features, it is considered the future of cell therapy, regenerative medicine, and anti-ageing medicine. It is still at its infancy stage, as clinical trials are underway.
Yet another breakthrough comes in the form of a polynucleotide, made out of Salmon DNA, which has the ability to improve the biological condition of damaged skin. It has self-rejuvenation properties, and a recent Korean study shows improvement in skin thickness, pores, tone, and tightness. In Korea, the product Rejuran® (Pharmareasearch Products, Inc., Seongnam, Korea) is widely used as a skin healer31.
Conclusion
In summary, injectables, with botulinum toxins and fillers, can be followed by skinboosters, PRP, and stem cells to optimize therapeutic efficacy. More research would be needed to identify the nature of combination, the sequence, timing, and number of sessions. Longer follow-up time and larger sample size clinical studies would help answer these questions.