Advantages of MRF
One of the greatest advantages of MRF is its application in all skin types26. Patients with Fitzpatrick skin types IV–VI have limited options for the improvement of acne scarring because of a greater incidence of post-inflammatory hypopigmentation (PIH), which most commonly appears 3–4 weeks after laser surgery14. Non-fractionated CO2 and Er:YAG lasers are indicated in skin types I–IV19, but up to 36% of patients (primarily skin types III and IV) can have PIH after non-fractionated ablative lasers21. The incidence of PIH varies greatly after laser treatment, ranging from 0–40% with non-ablative fractionated lasers21,28–30, and 0–15.4% with ablative fractionated lasers23,24,33,34. Differences in the energies, densities, number of treatments, number of passes, and Fitzpatrick skin types between studies influence this large variance in PIH.

Figure 2 Active acne and acne scar (left) before and (right) after three treatments with microneedle radiofrequency
All currently available fractionated lasers must be used conservatively in skin types IV and V, and are generally not advisable in skin type VI unless in the hands of an advanced laser surgeon22. It is advisable to decrease the fluence, density, and number of passes when treating darker skin types22,33,34. The epidermis sustains two-to-14-times as much damage with other available non-ablative and ablative fractionated lasers compared with fractional RF, leading to a higher incidence of dyspigmentation. No subjects treated with fractional RF displayed PIH26.
In another study25, there was a significant improvement in investigator-rated acne scarring, texture, and pigmentation. Patient satisfaction scores did not improve, although overall patient improvement scores did. It was speculated that the patients had higher expectations of the device on study entry. Although patients showed improvement, these high expectations were not met, as reflected in the lack of significant improvement in patient satisfaction scores. The fractionated bipolar RF device was better tolerated than the fractionated laser with RF device. Five treatments were administered every 30 days, but more treatment sessions may be required to produce more substantial clinical and patient-perceived results. Treatments every 5–6 months may be needed to achieve patient satisfaction in cases of acne scarring26.
Fractional radiofrequency with microneedling in active acne
MRF systems deliver energy directly to the dermis via a number of microneedle electrodes and create a microthermal zone (MTZ) providing untouched areas between MTZs. With the advantages of the fractional energy delivery system of MRF devices and evidence of cytokine alteration after treatment, comparable effect, less pain and less downtime can be expected compared with a non-ablative RF device in the treatment of papulopustular (inflammatory) acne vulgaris36.
Shin et al36 conducted a split-face comparative study between a fractional CO2 laser system (CO2 FS) on one side of the face and MRF on the other in 20 Asian patients suffering from active acne. They concluded that MRF and CO2 FS can be used for inflammatory acne vulgaris patients, and that it is more convenient than the CO2 FS because of its short downtime. They found that both devices — MRF and CO2 FS — were associated with moderate improvements in most patients, and the number of papules and pustules was significantly decreased in both sides of the face. However, there was no significant difference between the two treatment devices in terms of changes in papule and pustule counts. To get more than moderate improvement, multiple treatments might be necessary, as with other laser devices. In some patients, a dual benefit from the treatment was noticed; a decrease in acne lesions plus an improvement in previous scarring. However, the mean down time after CO2 FS irradiation was 11.8 days, which was five-times longer than the 2.4 days after the treatment with the MRF device. An attempt was made to treat patients twice with the same protocol, but most patients refused because of the down time and preferred to be treated with the MRF device. Transient hyperpigmentation was reported after CO2 FS treatment, although it spontaneously resolved within 3 months. This did not occur on the MRF treated side36.
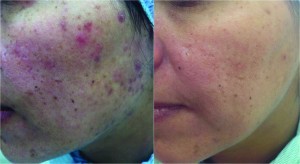
Figure 3 Active acne and acne scar (left) before and (right) after three treatments with microneedle radiofrequency
The possible mechanisms of the MRF device are similar to those of other lasers and light devices. Prieto et al37 reported that the combination of pulsed light and RF reduces the average areas of sebaceous glands and perifollicular lymphocytic infiltration. Hantash et al10 observed increases of TGF-β, MMP-1, MMP-13, HSP72 and HSP47 after fractional RF treatment, leading to neocollagenesis and neoelastogenesis. Cytokine alteration not only leads to extracellular matrix formation, but can also affect sebaceous glands. Ruiz-Esparza et al36 suggested that deep dermal heating with non-invasive RF treatment might inhibit the activity of sebaceous glands and stimulate dermal remodelling. Collectively, these results can explain the effects of the MRF device on both scarring and active acne lesions.
Conclusions
Treatment of acne and post-acne scars is considered a significant challenge in the field of aesthetic services in general, and in patients with darker skin in particular. The technology of microneedling with fractional RF might be a good step forward owing to efficacy and safety of the procedure in all skin types. Different mechanisms of action of this technology have been proven, such as new collagen synthesis shown in the histopathological studies mentioned earlier (others are still in the phase of speculation). However, a number of studies are ongoing to clarify further mechanisms of action, as well as further indications.
The authors are currently studying the effect of MRF in stretch marks alone and in combination with topical hyaluronic acid to evaluate its efficacy. In addition, the authors are conducting a study on enlarged pores to evaluate the efficacy of MRF. Both studies have had very good initial outcomes. The authors are now in the follow-up phase to evaluate the long-term efficacy of MRF.



