With the advent of fractional laser skin resurfacing, the number of completely ablative resurfacing cases has declined for most practitioners. However, care should be taken when treating sensitive areas such as the eyelids, upper neck, and especially the lower neck and chest, by using lower energy and density, as scarring has been noted in these areas25. Scarring after fractional CO2 laser therapy is considered mainly a result of overly-aggressive treatments and a lack of technical finesse. Physicians have also recorded post-operative infections leading to scarring, although it is generally felt that these may be prevented by careful history-taking, vigilant post-operative monitoring, and/or the use of prophylactic antibiotics26, 27.
With regard to facial rejuvenation, CO2 laser light at a 10600 nm wavelength results in vapourisation with thermal denaturation of type I collagen, collagen shrinkage and later, collagen deposition. However, in very deep rhytides, acne scarring and severe elastotic changes from sun damage, fractional CO2 therapy requires multiple treatments to achieve the same results as the older lasers28. A number of studies have evaluated using different laser combinations in the same session in order to improve collagen deposition, with a wider zone of fibroplasia6–9, 28. Owing to the inherent risks of fractional laser skin resurfacing and its inability to deal with some evidence of chronological ageing, it was advocated to here establish the clinical effectiveness of using a multi-procedural approach to volumisation and collagen regeneration. The author used microneedling with low energy laser, and platelet rich plasma (PRP) to address these issues.
Collagen remodelling and fibroblast stimulation
It is recognised that the most important rejuvenation process for photoaged skin is the collagen remodelling process, and dermal fibroblasts are known to have the most important function29. Rejuvenation of skin injury caused by UV light is a complex process that organically involves cytokines interacting with a number of growth factors and control proteins28. The procedures evaluated included PRP, microneedling, and Omnilux 633 nm near-red light, with neurotoxins as an adjunct to low-level fractional laser skin resurfacing. Cells in the epidermis and dermis can be targeted by microneedling and near-red light, resulting in fibroblast stimulation. Omnilux Revive™ (633 nm) therapy stimulates fibroblast activity, leading to faster and more efficient collagen synthesis and extracellular matrix (ECM) proteins. It also increases cell vitality by increasing the production of cellular adenosine triphosphate (ATP) and stimulates the contractile phase of the remodelling process producing better lineated collagen30–33. Collagen induction therapy is an aesthetic medical procedure that involves repeatedly puncturing the skin with tiny, sterile needles. Typically, this is done with a specialised instrument called a microneedling device.
Controlled studies have suggested that the application of autogenous PRP can enhance wound healing in both animals and humans29. Five major growth factors such as transforming growth factor (TGF), insulin-like growth factor (IGF), platelet-derived growth factor (PDGF), epidermal growth factor (EGF), and vascular endothelial growth factor (VEGF) are known to be related to the wound-healing processes28. These growth factors are released from platelets, and the production of collagen and fibroblasts is stimulated by IGF, EGF, Interleukin-1 (IL-1) and tumour necrosis factor (TNF)-α34, 35. In vivo studies report TGF-β to be the most stimulative growth factor. PRP may be used for dermal augmentation and Sclafani observed aesthetic improvements of the nasolabial fold in less than 2 weeks, and the results lasted for up to 3 months28, 29.
Research design and methods
This multi-centre randomised study included 44 patients of skin types 1 and 2 aged between 39 and 68 years, presenting with photoageing of the skin, 37 of whom were women and seven were men. The subjects presented with the typical hallmarks of chronological and photoageing, such as expression lines, rhytides, wrinkles, eyelid skin laxity, dermatochalasis, lowered brows, lateral hooding, and prominent fat pads. All patients were subjected to a programme of skin tightening and neocollagenesis by one of two methods: conventional fractional laser skin resurfacing (Group 1) or the DUBLiN Lift (Group 2). The mean patient age in Group 1 was 49 years (range 37–71 years) and in Group 2 was 55 years (range 41–76 years).
Fifteen patients underwent Lumenis ActiveFx™ with settings as (energy) 125 mJ and (rate) 19 w CPG 3/5/4. Twenty-nine patients received the DUBLiN Lift, a three-phase combination of established treatments with microneedling, platelet growth hormones, near-red 633 nm light, and low-energy UltraPulse fractional CO2 laser skin tightening. All patients received Dysport® in three areas 1 week prior to the other treatments as an adjunct to the laser resurfacing.
The DUBLiN Lift was introduced as three phases over a period of 3 weeks. Phase 1 included Dysport® at dilution 3.5 : 1 to three areas — glabellar, frontalis and periorbital. Phase 2 introduced intense fibroblast stimulation and modification through microneedling, PRP growth factor induction, and near-red phototherapy. Phase 3 administered the low–level (CO2) UltraPulse laser at 100 mJ 14 w CPG 3/5/2, and adjunct near-red 633 nm phototherapy. The study evaluated post-procedural aesthetic results at 2 weeks, 4 weeks and 12 weeks. The length of downtime, patient discomfort and adverse side-effects were noted for each phase.
Clinical assessment of patients in each group was made at 2 weeks, 1 month and 3 months post-operatively in the presence of two aesthetic staff. The degree of improvement in photoageing was based on the degree of re-epithelialisation rate, reduction of rhytides, reduction of tactile roughness, and loss of hyperpigmentation and telangiectasias. The prolongation and severity of erythema as well as the presence of negative side-effects (e.g. herpes) were also recorded.
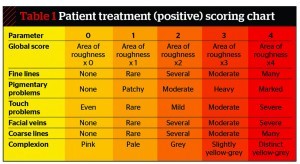
The efficacy of treatment was evaluated using a variation of the five-point scale (Table 1) originally suggested by Dover et al36. Investigators and patients evaluated efficacy using palpability assessments and change from baseline score at 0, 6 and 12 weeks. A total global score was recorded in each patient based on the addition of points obtained from six photodamage variables. The degree of perceived improvement in overall aesthetic effect reflecting chronological age was assessed separately by patients and physicians using the Wrinkle Severity Rating Scale (WSRS) and the Global Aesthetic Improvement Scale (GAIS). The WSRS is recognised as a valid and reliable instrument for quantitative assessment of facial skin folds, with good inter- and intra-observer consistency5. Wrinkle severity is measured using a wrinkle severity rating scale with 1 being absent and 5 being extreme. By allowing objective grading of data, these proved useful clinical tools for assessing the effectiveness of facial volumisation with PRP and microneedling–633.