Diagnosis of insulin resistance
It is imperative to make an early diagnosis before IR becomes decompensated. In fact, identifying cases where a disease is not yet apparent is important to prevent high mortality from cardiometabolic syndrome. Signs of IR could help to identify potential cases of an under-diagnosed condition.
In personal history we are looking for the following signs: specific ethnicity (Hispanic, Native American, east Asian), hypoglycaemic episodes and carbohydrate cravings, obstructive sleep apnoea, history of gestational diabetes, and menstrual irregularities in females.
A physical exam will find a range of ‘non-typical’ signs often presented as aesthetic concerns in aesthetic clinics, such as abdominal obesity, adult-onset acne, hirsutism, male pattern alopecia, gynaecomastia, and acanthosis nigricans. Nevertheless, each individual with abdominal obesity should have an initial check-up for IR: lipids level, fasting glucose, and HbA1c readings.
A Norfolk cohort prospective study26 showed the concentration of HbA1c significantly predicted mortality, independent of other common risk factors — even below the threshold commonly accepted for diagnosis of diabetes. Excess mortality was associated with HbA1c concentrations above 5% and predictive value for total mortality was stronger than the one documented for cholesterol, BMI, and hypertenson26. HbA1c has been checked in conventional medicine only in patients already taking anti-diabetic medication, and not as an initial check. Checking lipid levels can give some very important insights, especially the triglyceride/high density lipoprotein (TG/HDL) ratio, which is a simple test for IR:
- TG/HDL ≤ 3.0 normal — no IR
- TG/HDL ≈ 5.0 — suggestive of IR
- TG/HDL ≥ 8.0 — diagnostic of IR.
With these three parameters in combination with hypertension in individuals with abdominal obesity, a practitioner should ask the following questions: ‘Is it IR at all?’ And, ‘Is it compensated or non-compensated?’ Additional tests such as fasting insulin/glucose, postprandial glucose, and postprandial insulin can then be ordered for the full evaluation of the condition. It is interesting to mention that high fasting insulin concentrations appear to be an independent predictor of ischaemic heart disease in men.
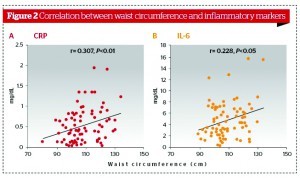
Since IR has an effect on almost all tissues in the body through mitochondrial toxicity, endothelial toxicity, and endocrine deregulation, one can only imagine the variety of the additional tests to be done for accurate diagnosis: CRP, cortisol levels, thyroid function, liver function test, CVD profile, oestrogen, progesterone, testosterone, and insulin-like growth factor (IGF)-1.
Integrative medical approach in treating IR
An emerging body of evidence27–32 suggests that the best results are achieved if the treatments are started early while IR is still in the compensated phase and an integrative medical approach is applied as following:
- Lifestyle interventions: dietary changes and weight management; exercise; stress management; POPs management (smoking cession, organic food, and support liver detoxification)
- Macro- and micro-nutritional management
- Botanical and phytonutrient supplementation.
Lifestyle interventions
In a study of 3234 non-diabetic subjects with high postprandial glucose, the lifestyle intervention reduced the incidence of progression to diabetes by 58% versus the metformin reduction of 31% (compared with placebo)27, revealing the importance and superiority of lifestyle changes.
Dietary changes are one of the most important long‑term interventions. Adequate carbohydrate intake with low GL, high fibre, and good fats are essential.
Dietary GL is defined as the product of a food’s glycaemic index (GI) and its carbohydrate content. The GL allows the assessment of the quantity, as well as the quality of the carbohydrate intake in the diet. In some studies28 there was a significant negative relationship between serum HDL cholesterol concentration and the glycaemic index of the diet for both men and women. Dietary GL is a stronger predictor than dietary fat intake of serum HDL cholesterol concentration. A decrease of 8% HDL cholesterol is associated with a 12-unit increase in the GI28.
There have been approximately 40 published studies examined GI on a variety of metabolic endpoints in a period from 1981–2002, of which 35 reported results support the use of the GI concept. Taken as a group, a reduction of the dietary GI by an average of 8–40 units reduced HbA1C by 9%, urinary C-peptide 20%, and triglycerides by 19%.29 Additonal support shows that plasminogen activator inhibitor-1 (PAI-1) was normalised on the low GI diet, showing a 54% decrease compared to the high GI diet30. Low GL dietary suggestions for the long term management of IR are:
- Total glycaemic load < 80 daily
- Each meal should have a glycaemic load of 20 or less
- Each snack should have a glycaemic load of 10 or less.
The GI and GL values of over 750 foods have been determined. The physician must supply the patient with a list of low GL foods since these are the most important for reversing IR.
It has been shown that low fibre is a risk factor for the development of type 2 diabetes31. The high fibre diet reduced total plasma cholesterol concentrations by 6.7%, triglyceride concentrations by 10.2%, and very low-density lipoprotein (VLDL) concentrations by 12.5% as well as 24-hour plasma glucose and insulin concentrations by 10% and 12%, respectively.
The right balance of saturated, polyunsaturated, and monounsaturated fats is important both for the prevention and treatment of diabetes. Saturated fats should be less than 10% of total calories. Total fat intake should be less than 30%. There is no evidence that high monounsaturated fat diets stimulate weight gain in patients with type 2 diabetes given that energy intake is controlled.
Exercise has been advocated by conventional medicine in all patients with type 2 diabetes, but it is accepted as an early intervention for the prevention as well as treatment of IR. Meta-analysis on exercise in type 2 diabetes suggests exercise training will reduce HbA1c, even without a change in body weight32. Moderate, consistent aerobic exercise (increases resting metabolic rate and burns fat) and resistive exercise (increases muscle mass) are highly recommended.
Nutrients known to modify insulin responsiveness at the cellular level are:
- Chromium 1000 mcg/day33
- Alpha-lipoic acid 600 mg34
- CoQ10 100–200 mg35,36
- Vitamin D 2000–4000 IU daily20
- Magnesium 200–400 mg37
- Vitamins C, E, and other antioxidants38
- Omega-3 fatty acids 2 g39
- Vanadium 1–2 mg long term40.
It is advisable to prescribe the above nutrients in modifying insulin responsiveness only in the case of underlying deficiencies. There is much evidence documenting nutrient deficiencies in a modern society diet41,42. Among US adults, 68% consume less than the recommended daily allowance (RDA) of magnesium, and 19% consume less than 50% of the RDA. Approximately 90% of the diets analysed were below the minimum suggested safe and adequate daily intake of 50 mg for chromium, and magnesium and vitamin C intakes were low in more than 50% of the sample. Vitamin D inadequacy has been reported in approximately 36% of otherwise healthy young adults in the US and up to 57% of general medicine inpatients. It is an even higher percentage in Europe, and more than 80% in South Africa43.
Phytonutrient recommendations
Recommendations cover a range of different ingredients, including:
- Green tea Consume 200 mg or more daily. Green tea decreases glucose production in the liver, decreasing hyperglycaemia, and protects beta cells as a potent antioxidant44
- Cinnamon Consume 1 g daily. Cinnamon increases insulin receptor ‘receptiveness’ in skeletal muscle, increases glucose uptake and use in a skeletal muscle, and decreases beta cell distraction45
- Fenugreek Consume a somewhat impractical 15 g per day. Decreases small intestine digestion of polysaccharides46
- American ginseng Decreases small intestine digestion of polysaccharides. Variable effects can be experienced depending on exact ginsenoside profile47
- Banaba Positive action on insulin receptor or as alpha-amylase inhibitor, as well as increasing glucose uptake and use by skeletal muscle. The specific dose has currently not been studied48.
Methods to decrease visceral fat and lower Inflammation, include:
- Fish oils 2 g/daily49
- Boswellia 400 mg three times per day50
- Curcumin 300 mg twice per day51
- CoQ10 100 mg daily35
- Exercise32
- A low GL Mediterranean diet.
Conclusions
The danger of abdominal fat has been well researched and has moved beyond the point of being seen as just an aesthetic problem. It correlates with visceral fat that is metabolically active and associated with IR. Reactive hyperinsulinaemia and underlying inflammation are involved in the cascade process of developing cardiovascular disease, type 2 diabetes, cancers, and PCOS, which are in alarming epidemic proportions. Focus should be on identifying individuals who are insulin-resistant for an aggressive targeted intervention, mostly through long-term lifestyle changes.