Diane Irvine Duncan presents six cases of scarless breast lifting using an energy-based approach
The inevitable decline in the attractiveness of female breasts over time has been attributed to childbearing, weight loss, and simple aging. The perception that loss of skin elasticity is the root cause of sagging breasts is just not true. Those of us that perform breast surgery know that the framework upon which the skin hangs is much more important. The skin follows the scaffold underneath. A lack of a cohesive form under the breast skin translates into a poor shape.
While facial aging tends to become noticeable in the mid-40s, mammary ptosis can become significant as early as the mid- to late-twenties. There is no diet or exercise program that will improve the appearance of deflated or ptotic breasts. Until recently, the only two viable solutions for improvement have been the placement of breast implants to fill out the skin envelope, and/or surgical skin excision, also known as mastopexy. Limitations of breast augmentation include the unavoidable side-effect of larger breasts, and the ever present possibility of residual ptosis if the skin envelope is so large that implants alone will not correct the problem. Difficulties with surgical breast lifts include visible and sometimes unattractive scars, the possibility of permanent numbness, and recurrent drooping despite significant skin excision. Large nipple-areolar diameters are rarely corrected with a periareolar mastopexy. Bottoming out is a frequent late sequela of a ‘lollipop’ or Lejour type mastopexy. Anchor pattern mastopexy can have significant post-op scarring, numbness, and a ‘boxy’ look if the medial and lateral and axillary aspects are not adequately addressed.
The origin of energy based breast lifting in 2007 has been noted as a major advance in treating the ptotic breast, as the technique directly addresses the root cause of soft tissue laxity in the breast region: the lack of collagen binding fibrils holding the adipocytes and glandular tissue together in a defined shape.
History of scarless breast lifting
Guillermo Blugerman performed the first known scarless radiofrequency assisted breast lift in Argentina in December of 2007, using a bipolar RF device to tighten the subdermal tissue1. Duncan began using a similar device to perform subcutaneous soft tissue heating resulting in tightening of the skin envelope in conjunction with breast augmentation in 20092,3.
Becker, in 2011, announced the development of a subareolar dermal mesh procedure as a ‘scarless’ mastopexy4. This work, published in 20135, clearly describes the use of periareolar incisions that the author claims are ‘invisible’.
Khouri developed a scarless procedure reported in February 2013. The procedure uses a needle type device to separate the breast skin from the underlying parenchyma, and then fat grafting is performed. The patient then wears a support device called the ‘PexyBra’ to hold tissues in place as they heal6. No surgical incisions were used.
In 2014, Fisher began using a barbed thread called ‘refine’ to resuspend the breasts, creating more upper pole fullness7.
While many physicians purport that their method of breast lifting is scarless, most of the techniques described above use such approaches as a standard breast augmentation8, avoid the vertical incision, or avoid using an inferior incision in the case of a Lejour type approach. In 2016, DiBernardo presented the use of a monopolar radiofrequency device for the purpose of breast lifting9. Other truly scarless options include the use of micro-focused ultrasound10 and external radiofrequency heating.
The needs being addressed among patients using this energy-based approach include primary breast lifting for those patients with ptosis who don’t want larger breasts, as well as for those undergoing breast augmentation who also need skin envelope reduction. In selected patients with existing breast implants, large implants can be removed and smaller ones placed in combination with skin envelope reduction using radiofrequency-assisted subcutaneous tissue heating. Other uses for RF assisted breast lifting include primary breast reductions in combination with liposuction, correction of bottoming out, and improvement of tissue migration over time in patients who already have breast implants. Improvement of asymmetry is a common use of the technique as well.
Case reports
#1 Optimal patient: primary breast lifting
History
A 35 year-old with one child that she breast fed. She noted a lack of upper pole fullness, a lax and ‘folded over’ contour, and asymmetry with ptosis more prominent on the right. Initial bra size was 34B. She did not desire larger breasts.
Reason for choosing this treatment
She would decline treatment if traditional surgery with incisions was the only solution. She desired improvement in tissue flaccidity, which is not achieved with mastopexy.
Treatment goals included improvement of ptosis and asymmetry, more tissue firmness, and more defined cleavage.
 Method and result
Method and result
Pre-operative documentation of the patient’s condition included 2D and 3D Vectra (Canfield Scientific, Inc., NJ, US) photographs, and physician based measurements. The procedure was performed under light general anesthesia. The tumescent infusion was placed in the subcutaneous tissue, and the access points were created with an 18 gauge needle. The Silk’n FaceTite device (Home Skinovations Ltd., Yokneam, Israel) was used to heat the breast region, making sure to treat all areas. A postoperative brassiere was worn for support.
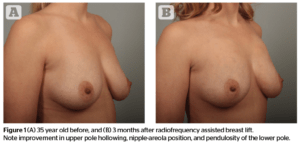
Figure 1 shows the patient’s appearance before and 3 months after treatment. Lower pole pendulosity was greatly improved with this treatment. The ‘long breast’, common after breast feeding, is improved with the RF based approached. Note the far breast no longer rests on the lower chest wall. The nipple is lifted and upper pole hollowing is improved.
#2 More challenging patient
for primary breast lifting
History
This 28-year-old gave a history of going through puberty at age 11. She developed moderately large, pendulous breasts and was quite self-conscious. Her preoperative bra size was 34 DD.
Reason for choosing this treatment
She was hoping for a lift but strongly disliked the idea of permanent scars. She was self-conscious about the size of her breasts and declined several offers by other surgeons to give her a lift combined with implant placement.
 Method and result
Method and result
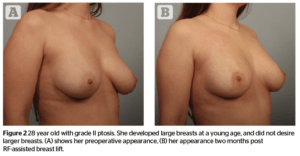
Pre-operative documentation and treatment technique was similar to that of case 1. Figure 2 shows her appearance before, and 6 weeks following treatment with RF assisted mastopexy. The degree of improvement in this patient is remarkable and not usual. She is young and was very good about wearing her support garment. Significant contraction of the soft tissue and overlying skin can be seen in this case.
#3 Breast augmentation
plus simultaneous RF-assisted lift
History
This 32-year-old noted post-partum ptosis and loss of volume, especially in the upper pole. She wanted larger breasts but was concerned that her breasts might still be ptotic with an implant alone.
Reason for choosing this procedure
The patient declined traditional periareolar mastopexy as she wanted the fewest external scars possible.
 Method and result
Method and result
Pre-operative documentation included 2D photographs and physician based measurements. Operative technique was similar to that of case 1, followed by a dual plane breast augmentation with an inframammary approach. 360 cc moderate profile gel implants were used.
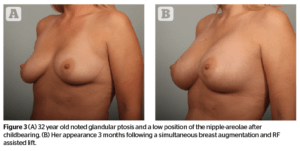
Figure 3 shows her appearance before surgery and at 3 months postoperatively. The most common indication for this procedure is enhancement of a breast augmentation when the nipples are low. If the areola extends to the visible lower margin of the breast, a lift is indicated. Results in case 3 show the nipple position in the center of the breast, and no breast skin touching the upper chest.
#4 A more challenging patient desiring
both a scarless breast lift and augmentation
This 30-year-old had two children in rapid succession and breast fed them both. She had grade III ptosis and was told she was not a candidate for the RF based procedure.
Reason for choosing this procedure
She continued to decline traditional mastopexy. After several consultations, I agreed to perform the RF procedure first and recommended that the patient waits 6 months before having a breast augmentation, so the optimal lift is achieved without the added weight of an implant. The patient agreed to the two stage procedure.
 Method and result
Method and result
Preoperative documentation included 2D and 3D photographs and physician based measurements.
Operative technique was similar to that of patient #4, although the procedures were performed at two separate time periods. During the second procedure, she had 340 cc moderate profile implants placed subpectorally.
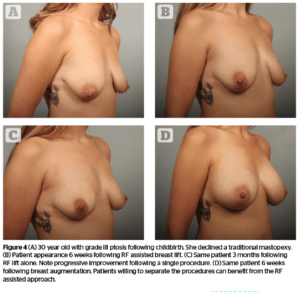
This patient had severe ptosis and would not normally be treated with an RF lift. She declined traditional surgery. Figure 4 shows the patient before her surgery, at six weeks and 3 months post RF lift, and again six weeks following her dual plane breast augmentation. While the result was not ideal, the patient was very pleased with the level of improvement she achieved. Her results are good because she underwent the RF lift first, then had an augmentation as a second stage. While her nipples are still a bit low, her result shows a good contour.
#5 Removal of larger breast implants and replacement with smaller implants
History
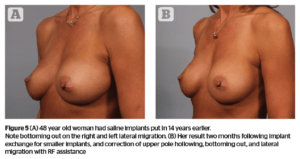
This 48-year-old patient had saline implants placed in the subpectoral position 14 years prior to her return visit.
Reason for choosing this procedure
The patient stated that she had gone back to graduate school and felt that the look of her breasts did not fit the professional image she wanted to project. She noted bottoming out on the right and lateral migration on the left. She originally had 350 cc saline implants, slightly overfilled, and wanted to reduce the size to 275 cc.
 Method and result
Method and result
Preoperative documentation included 2D photographs and physician based measurements.
Operative technique was similar to that of patient 1, followed by saline implant removal, superomedial capsulotomy and inferolateral capsulorrhaphy (thermal capsular shrinkage), and implant replacement with 275 cc gel moderate profile implants.
Figure 5 shows the patient before the procedure and 2 months post-op. This patient had excellent correction of right bottoming out and left lateral implant migration following her procedure, replacing her larger implants with a smaller size.
#6 Performing both a lift and smaller implants
History
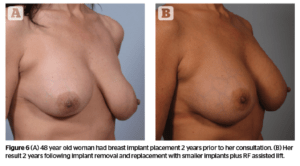
This 48-year-old patient with a bigger challenge had primary breast augmentation performed 2 years prior to her consultation in a different city. She disliked the residual ptosis and asymmetry. She also felt her breasts were too large, especially on the left.
Reason for choosing this procedure
She wanted both a lift and smaller implants. She had declined a traditional surgical mastopexy with her first surgeon and declined again any mastopexy that would result in more scars. Her original implants were 425 cc gel implants.
 Method and result
Method and result
Preoperative documentation was 2D and 3D photographs plus physician based measurements.
The surgical technique was similar to that of patient 5. New implants placed were 350 cc moderate profile gel implants. It was found that the left implant had migrated inferiorly and was no longer subpectoral, so that pocket was corrected. The RF heating was performed first, then the implant removal and replacement immediately followed within the same surgical session. Due to the asymmetry, more RF energy was used on the left side.
This patient had asymmetry and severe left ptosis. She wanted smaller implants and a significant lift. Figure 6 shows the patient before surgery and again two years following the combined RF lift and implant replacement procedure. Results show a significant improvement persisting for 2 years following treatment.
Discussion
The biggest drawback of the procedure is the limitation of aesthetically pleasing soft tissue contraction to about 33% of the original skin surface area11. Upon review of the author’s 319 cases of radiofrequency-assisted breast lifting, the average clinical response was improvement of a single grade of ptosis. Patients are counseled that pursuing the RF-assisted scarless lift will, in most cases, give less nipple–areolar lift than a surgical mastopexy. However, significant aesthetic reduction of the overall skin envelope can usually be achieved. Because the mechanism of action is generation of a multilayered new collagen framework within the subcutaneous layer, more tissue firmness is achievable than with skin excision alone. Upper pole fullness can be restored to a moderate degree in patients undergoing an RF lift alone. Strong clinical improvement in bottoming out is achievable using this technique. While spot treatment can be helpful in some cases, best clinical results are achieved when the entire skin envelope is treated.
No patients were nonresponders, but about 5% noted they did not see as much improvement as they hoped to have seen. One patient had the procedure repeated 8 years later for recurrent unilateral ptosis.
Expected sequelae can include temporary numbness or hypersensitivity, temporary subcutaneous nodularity, and less than hoped for improvement in ptosis. Unexpected sequelae could include hematoma, infection, unsatisfactory scars at the needle access points, and burns.
None of these were noted in this series. As the tumescent infuser and RF heating device measure 1.8 mm in diameter, an 18 gauge needle can be used without the need to make the access port larger. While the procedure does not leave permanent visible scars, the needle access ports do make this non-excisional technique minimally invasive instead of noninvasive.
Conclusion
The radiofrequency-assisted scarless breast lift is a relatively new and uncommon procedure. While patient acceptance is high, the possibility of unmet expectations is also high. Therefore during the initial consultation, the limitations of the procedure should be clearly explained. The ideal patient is a younger patient with B to C cup breasts, who does not need more than one level of ptosis correction. Contraindications for treatment with RF breast lifting include patients with grade III or IV ptosis, large pendulous breasts, inability to follow postoperative recommendations, and unrealistic expectations regarding the degree of improvement that can be obtained.