Steven Harris explains how the discovery of Ruffini-like structures in the zygomaticus muscles could lead to greater understanding of muscle activity after a filler injection and potential for a new approach to facial aesthetics
Myomodulation refers to the change in muscle activity that occurs when a dermal filler is injected next to it. The process is very commonly observed in non-surgical facial aesthetic procedures, but its underlying mechanism is not fully understood. A number of attempts have been made to try and explain the phenomenon ranging from changes associated with simple laws of mechanics to stimulation of cutaneous mechanoreceptors1–4. However, to date all the explanations fail to present a coherent and comprehensive account of the change in behaviour in both elevator and depressor muscles. A recent finding of Ruffini-like structures in the zygomaticus major muscle is the key to a more complete understanding of the underlying mechanism5. It suggests that placement of a filler next to a muscle may stimulate mechanoreceptors within the muscle itself to involve the Autonomic Nervous System (ANS) in changing not only the particular muscle’s activity but that of all the facial elevator and depressor muscles, including a reduction in emotional arousal.
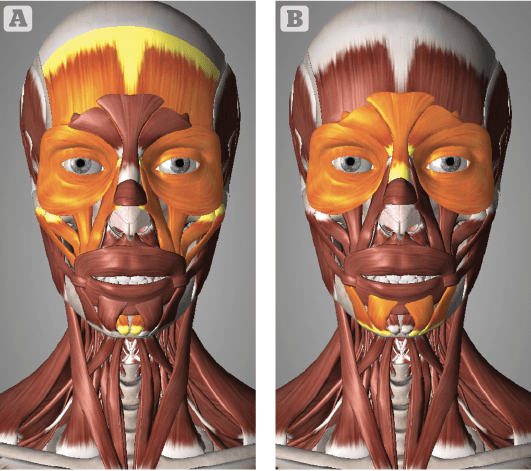
Figure 1 The elevator muscles (A) and depressor muscles
(B) of the face. The Orbicularis Oculi has both elevator and depressor activity. Printed with permission from 3D4Medical: www.complete-anatomy.com
Myomodulation is very commonly observed in facial aesthetics involving dermal fillers. When a filler is injected deep to any of the elevator muscles of the midface or lower face it appears to increase not only the contractility of the particular muscle, but all the elevators while inhibiting that of their depressor opposites. A filler placed deep to the midface elevator zygomaticus major not only stimulates this muscle, but also the zygomaticus minor and levator labii superioris (LLS) as well as the lower face elevator mentalis. At the same time, the depressor section of orbicularis oculi, depressor anguli oris (DAO) and depressor labii inferioris (DLI) appear to all be inhibited. When the filler is injected under one of the depressor muscles, the same changes occur; the activity of all the depressor muscles is inhibited while that of the elevators is stimulated. In contrast, if the filler is injected above any of the muscles, then it acts to inhibit the effect on the particular muscle’s activity1. While the activity of all the elevator and depressor muscles of the face are predictable in this way, the contractility of the elevator muscle, frontalis is apparently inhibited, not stimulated when a filler is placed under it.
Mechanism of myomodulation
The challenge then is to understand what underlying mechanism could account for all these changes which on the face of it (no pun intended) appear to be inconsistent. A number of explanations have been proposed; the most recent and perhaps the most ambitious by Mauricio de Maio. De Maio attempts to explain the mechanism of myomodulation in terms of age-related changes to the muscles themselves, which, according to him, stretch and elongate over time altering their ideal resting length for effective contraction. The filler placed under the stretched muscle would act as a pulley to modify its length-tension relationship and in line with the Frank-Starling law of mechanics contract more effectively. According to de Maio, filler placed above the muscle mechanically compresses it downward to reduce its contractile functioning2.
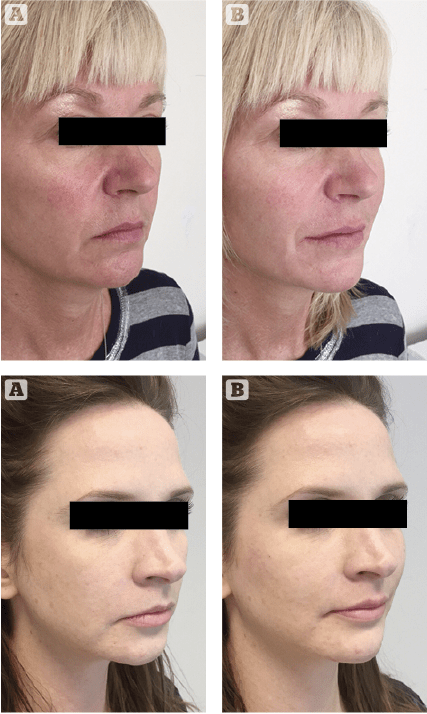
Figures 2 & 3 Dermal fillers placed deep to the elevators, zygomaticus major and mentalis and the depressor muscle, DOA resulting in a net elevator effect with a parasympathetic shift in emotional appearance. (A) Before, (B) after
Indeed, as Kane points out, there is some merit to this explanation in that fillers placed deep to the mid-face elevator muscles would function more effectively from their newly supported and raised position, but it does not account for the behaviour of the elevator frontalis, nor does it explain the behaviour of the depressor muscles. Also, a filler injected superficially exerts pressure in all three dimensions rather than just downward onto the muscle. According to Kane, a more plausible explanation is that the superficially placed filler reduces the ability of the dermis to deform, thereby indirectly reducing the contractility of the underlying muscle. Moreover, he goes onto explain there is no evidence to support the idea that muscles elongate over time and that the elevators weaken more than the depressors. If anything, it is more likely that both the elevators and depressor muscles shorten and weaken during the ageing process along with the contracting skull and soft tissues1.
Mechanoreceptor filler hypothesis
The proposal here is that the recent discovery of Ruffini-like corpuscles in the mimetic muscles offers a more plausible and comprehensive explanation of the underlying mechanism of myomodulation. The mechanoreceptor filler hypothesis states that a filler placed next to a facial mimetic muscle causes a mechanical deformity to stimulate slow adapting mechanoreceptors in the muscle itself. These, in turn, signal the brain via autonomic and somatosensory pathways to decrease sympathetic arousal associated with depressor muscle activity in favour of more parasympathetic activity associated with elevator muscle activity. The contraction of the frontalis is a sympathetic activity and, therefore, unlike the other elevators, it is inhibited. The hypothesis also explains a reduction in emotional arousal due to the decrease in sympathetic activity and why patients often appear more emotionally relaxed following treatment with fillers. In terms of superficial placement of filler, it is more likely that the underlying mechanism is a result of Kane’s explanation; reduced muscle activity simply due to a dermis less able to deform.
Over 17,000 sensory receptors have been reported in the human face. The response of the face to touch or indentation of the skin is mediated by facial cutaneous mechanoreceptors located in superficial layers of skin6. These may be divided into slow adapting (SA) receptors firing with constant indentation of the skin and rapidly adapting (RA) receptors responding only to the onset and offset of indentation7. SA Receptors include Merkel cell discs (SA1), Ruffini corpuscles (SA2) and free nerve endings (10% thinly myelinated, SA3 and 90% unmyelinated, SA4). Free nerve endings are the most common mechanoreceptors in the face and may be further divided equally into low-threshold pressure (LTP) units responding to light touch and high-threshold pressure (HTP) units responding to deep touch. RA receptors include Meissner corpuscles (RA1) and hair receptors (RA2)7,8.
It appears that stimulation of SA receptors involves not only the somatosensory pathways but also the autonomic nervous system (ANS). The trigeminal nerve which carries sensory information to the central nervous system (CNS) is accompanied by both sympathetic and parasympathetic fibres along its course6,8. Indeed, stimulation of SA receptors is associated with pleasurable touch sensation as well as the lowering of sympathetic activity via an autonomic loop6. According to the model of hypothalamic tuning, this increased vagal activity leads to a more trophotropic hypothalamus via a second autonomic loop9. The result is a decrease in sympathetic muscle tone and a reduction in emotional arousal, thereby activating elevator muscles associated with a parasympathetic response and inhibiting depressor muscles (and the elevator frontalis) associated with a sympathetic one, all while promoting emotional relaxation. Indeed a study by Harris et al. found that when facial cutaneous SA mechanoreceptors were stimulated with small silicone projections on an eye-mask, the glabella lines (caused by depressor muscle activity) were reduced significantly by 64% after a period of 15 minutes. The subjects also reported an improvement in mood3.
Sensory system in facial muscles
While the sensory receptors of skin are well documented, less is known about the underlying intrinsic sensory system of the facial muscles5. The motor functions of the muscles of facial expression are controlled by the efferent fibres of the facial nerve (CNVII) while proprioceptive information is gathered by the afferent sensory nerve fibres of the trigeminal nerve (CNV) and its three major branches: the ophthalmic nerve (V1), the maxillary nerve (V2) and the mandibular nerve (V3). Neuroanatomical studies have demonstrated multiple branch communications between the trigeminal and facial nerves as the former makes its way to the mesencephalic trigeminal nucleus for processing, but there is no common agreement on the function of these nerve fibres. Some have suggested that the relationship is merely ones of contiguity while others have suggested that the communicating rami convey proprioceptive information regarding the mimetic muscles11. According to Baumel, sympathetic and parasympathetic fibres, not belonging to the trigeminal nerve, may also be the constituents of the communicating rami12.
The receptor organs for striated muscle proprioception, muscle spindles, operate essentially as stretch receptors, but it is widely accepted that these are either very scarce or absent in the muscles of facial expression5. Kadanoff found evidence for a few spindles and other similar structures in some facial muscles, but noted that they were aberrant in form and not sensory in nature13. Dubner et al. have suggested that deep cutaneous mechanoreceptors are sensitive to skin movement brought about by the contraction of facial muscles, but according to Cobo et al. this ‘functional substitution’ has not been demonstrated5. In a recent study, Cobo et al. investigated whether other kinds of sensory structures were present in two human facial muscles (zygomatic major and buccal). The muscles removed from cadavers were processed for immunohistochemical detection of nerve fibres and two mechanoproteins associated with mechanosensing. Nerves of different calibres were found in the connective septa and within the muscle itself. In all the muscles analysed, capsular corpuscle-like structures resembling elongated or round Ruffini-like corpuscles were observed, and the axon profiles within these structures displayed immunoreactivity for both mechanoproteins5.
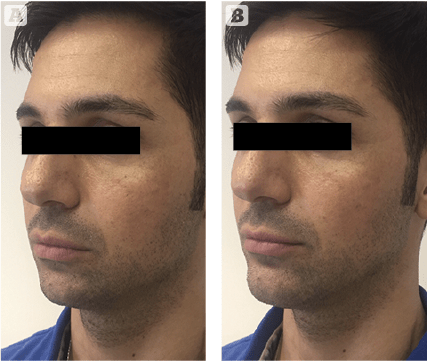
Figure 4 Dermal fillers placed deep to the elevator muscle, mentalis resulting in a net elevator effect and a parasympathetic change in emotional appearance. (A) Before, (B) after
The finding of Ruffini-like corpuscles acting as mechanoreceptors in the facial mimetic muscles forms the basis of the present mechanoreceptor filler hypothesis; it explains how fillers placed in the soft tissue of the face cause a deformity to stimulate mechanoreceptors in the mimetic muscles themselves. As explained above, stimulation of these mechanoreceptors leads to a cascade of events involving the CNS and ANS to create a disinhibition of the inhibitory sympathetic nervous system in favour of a parasympathetic one. Thus filler placed deeply near the insertion of the elevator zygomaticus major not only acts as a lever or pulley, but as an inhibitor of the sympathetic nervous system. The filler not only stimulates the activity of the muscle itself to raise the corner of the mouth but with the exception of frontalis muscle increases the activity of all the elevators over that of the depressors along with a reduction in emotional arousal. As a result, the mid-face and lower- face demonstrate a net elevator effect including the lateral brow with an overall improvement in definition, closer to the patient’s ideal facial shape and a more relaxed appearance (Figures 2–4).
The same series of events takes place when the filler is placed deep to one of the depressor muscles, for example DAO; its depressor activity along with all the other depressors is inhibited in favour of the elevator muscles to create not only a local improvement, raising the corner of the mouth, but improving the facial shape as a whole. As mentioned above, the contractility of the frontalis is associated more with a sympathetic response and therefore injecting a filler deep to it reduces its contractility. In these examples and injections involving all the other elevator and depressor muscles, the filler placed deep to the muscle not only leads to a physical change, but to a more emotionally relaxed appearance; a result of increased parasympathetic flow. Fillers placed superficially to any of these muscles merely inhibits the activity of the particular muscle, therefore exerting a more local effect rather than one involving the CNS.
Conclusion
The mechanoreceptor filler hypothesis offers a scientifically plausible and comprehensive explanation of myomodulation relating to fillers placed deeply and/or superficially to the elevator and depressor muscles of the face. It suggests that newly discovered mechanoreceptors in the mimetic muscles themselves are responsible for the observed changes. When stimulated by deeply placed fillers, these mimetic muscle mechanoreceptors are stimulated to initiate a series of events involving the CNS and in particular the ANS resulting in disinhibition of the inhibitory sympathetic nervous system to alter activity not only of the local muscle, but all the elevator and depressor muscles of the face. The overall effect is a net elevator one with an improvement toward the patient’s ideal facial shape while reducing emotional arousal toward a more relaxed appearance. The implications of the mechanoreceptor filler hypothesis in terms of non-surgical facial aesthetics involving fillers are significant. They suggest a new sophisticated understanding and approach to using fillers as myomodulators. The approach involves strategic placement of small amounts of filler typically deep to an elevator or depressor muscle anywhere in the face to cause not only local changes in muscle activity but changes involving all the elevator and depressor muscles toward restoring the ideal facial shape. This new ‘less is more’ holistic approach not only works toward achieving physical change but aims to reduce sympathetic activity toward a more emotionally relaxed parasympathetic appearance.
Declaration of interest None
Figures 1 © 3D4Medical; 2–4 © Steven Harris
References:
- Kane MAC (2018) Commentary on Myomodulation with Injectable Fillers: An Innovative Approach to Addressing Facial Muscle Movement. Aesth Plast Surg 42:1360–1363
- De Maio, M (2018) Myomodulation with Injectable Fillers: An Innovative Approach to Addressing Facial Muscle Movement. Aes Plas Surg 42(3): 798-814
- Harris S (2016) Reduction of glabellar lines using a silicone eye mask. Prime journal Nov Ed. 36-39
- Kane MAC (2005) The functional anatomy of the lower face as it applies to rejuvenation via chemodenervation. Fac Plast Surg 21:1–55
- Cobo JL, Francesco A, de Vicente JC, Cobo J, Vega JA (2017). Searching for proprioceptors in human facial muscles. Neurosci Lett (640) 1-5
- Siemionow M, Gharb BB, Rampazzo A. (2011) The face as a sensory organ. Plastic Reconstructive Surgery 127(2): 652-62
- Abraira V, Ginty D. (2013) The sensory neurons of touch. Journal Neuron 79(4): 618-639
- Schleip R. (2003) Fascial plasticity – a new neurobiological explanation. Journal of Bodywork and Movement Therapies 7(2): 104-116
- Gellhorn E. (1967) Principles of Autonomic–Somatic Integration: Physiological Basis and Psychological and Clinical Implications. University of Minnesota Press
- Cabo R, Alonso P, Vin E (2015) ASIC2 is present in human mechanosensory neurons of the dorsal root ganglia and in mechanoreceptors of the glabrous skin. Histochem. Cell. Biol. (143) 267–276
- Patestas M, Gartner L. Ascending sensory pathways (2016) A textbook of neuroanatomy, second edition. Wiley-Blackwell (12) 137-170
- Baumel JJ. (1974) Trigeminal-Facial Nerve Communications. Their Function in Facial Muscle Innervation and Reinnervation. Arch Otolaryngol. 99(1):34-44.
- Kadanoff D (1956) Die sensiblen Nervenendigungen in der mimischen Muskulatur des Menschen. Z. Mikrosk. Anat. Forsch. 62: 1-15.






