CO2 and IPL
Better results can be obtained with Er:YAG laser resurfacing and the combination of pulsed CO2 laser and QS alexandrite laser, as the CO2 laser destroys the melanocytes while the alexandrite laser removes the pigment left in the dermis. IPL is a non-coherent, broad-spectrum light source that emits a continuous spectrum in the range of 500 nm to 1200 nm. Its therapeutic efficacy is relatively higher in patients with epidermal melasma than those with mixed melasma29. This phenomenon could possibly be related to the location of the melanin. In epidermal melasma, the melanosomes in the epidermis rapidly migrate to the skin surface and shed off with microcrusts. In mixed melasma, the melanin-laden macrophages in the dermis are barely damaged30–31. In a 2010 study, Zoccali et al32 had excellent results with the use of IPL in melasma, they treated 38 patients (with Fitzpatrick phototypes III–IV) with IPL over three-to-five sessions at intervals of 40–45 days. They chose a 550 nm handpiece, since it offers great selectivity for melanin and reaches the deeper epidermis, using two pulses of 5–10 ms with a 10–20 ms delay between pulses, while the fluence was modulated with regard to the anatomic area. Energy levels of 12–14 J/cm2 were used to treat the cheeks and zygoma, 10–12 J/cm2 for the forehead, while lower levels (7–8 J/cm2) were used on the area around the eyes and neck. Results were excellent in 18 patients (47.37%), good in 11 (28.95%), moderate in five (13.16%), and poor in four cases (10.52%), in which a recurrence of hyperpigmented areas occurred within 2–4 months32. Side-effects were minimal and included a burning sensation during treatment and erythema for a short period. Possible complications included transitory hyperpigmentation, persistent hypopigmentation, and rarely, scarring.
A 10-week, split-face study by Goldman et al33 evaluated the safety and efficacy of TC cream when used sequentially with IPL in patients with moderate-to-severe melasma versus an inactive control cream associated with IPL at 2 and 6 weeks. The melasma area severity index (MASI) was significantly less with TC cream and IPL than with inactive cream and IPL at weeks 6 (P=0.007) and 10 (P=0.002), and the treatment was well tolerated, although cutaneous irritation was greater with IPL plus TC cream than with IPL plus inactive cream (P<0.25 for all assessments).
In the authors’ opinion, IPL can be considered a valid therapeutic option — particularly in non-responders to conventional topical agents — however, only temporary and transient results can be achieved as there is repeat onset of hyperpigmentation lesions after a few weeks or months.
Fractional resurfacing is a novel concept of skin rejuvenation that has the potential to treat a variety of epidermal and dermal conditions34. It produces a unique thermal damage pattern. In contrast to ablative skin resurfacing and non-ablative skin resurfacing, which achieve homogenous thermal damage at a particular depth, fractional resurfacing creates microscopic thermal lesions (i.e. MTZs)35–36. Fractional resurfacing specifically spares the tissue surrounding each MTZ, thus allowing for rapid re-epithelialisation and fast epidermal repair owing to the small size of the lesions and short migratory paths for the keratinocytes. In studies by Kroon et al, non-ablative 1550 nm fractional laser therapy proved to be a safe treatment option for patients with darker skin types when topical bleaching was ineffective or not tolerated37.
Niwa Massaki et al38 investigated the efficacy and safety of a single administration of a high-density fractional thulium fiber laser (1927 nm) at 10 or 20 mJ/cm2 for the treatment of refractory melasma in 20 patients. Mean MASI scores decreased dramatically from 13.2 ± 5.4 before treatment to 8.5 ± 3.5 at 4 weeks after laser treatment (P=0.004). Patient assessment revealed that 12 of the 20 subjects had more than 50% clearance of their melasma. Recurrence was reported in seven out of 15 patients who were successfully followed-up (mean 10.2 months).
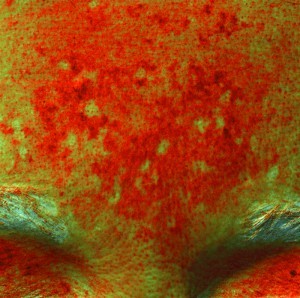
The biological role of cutaneous blood vessels in the pathogenesis of melasma is an interesting topic and opens new therapeutic perspectives. Recently, the authors performed a prospective study for evaluating the effects of pulsed dye laser (PDL) therapy. After a multispectral study for evaluating haemoglobin and melanin components, the authors are using this vascular laser with a low fluence and have obtained some notable improvements6–8. It would be tempting to think that the action of PDL on vascularisation might have played an important role in preventing relapse. By targeting vascularisation and at least some part of the elastosis in the melasma lesions, it might be possible to decrease the stimulation of melanocytes and thus reduce the incidence of relapse.
Conclusions
All the laser devices discussed in this article represent new horizons for the treatment of hyperpigmentation disorders, and particularly in darker-skinned patients (Fitzpatrick skin types IV–VI).The use of lasers and pulsed light in the treatment of benign superficial pigmented lesions has revolutionised the possibilities of therapeutic responses available for the dermatologist.
Physical treatment with lasers (especially IPL) is usually limited to those patients who fail to respond to primary topical and cosmetic treatment. However, in the authors’ experience — and particularly in the treatment of melasma — it is only possible to obtain transient results with the likely reappearance of hyperpigmented lesions. Physical methods using lasers sometimes yield rebound hyperpigmentation.
The importance of the role of vascularisation in the pigmentation process must be studied further. This field of research may provide new therapeutic options, such as vascular lasers or anti-angiogenic agents. It is essential to carry out a precise clinical, dermatoscopic and multispectral evaluation of the hyperpigmentation in order to select the most appropriate treatment and ensure adequate post-treatment care (photoprotection) and follow-up, as well as the quality and maintenance of results.