As women are now living longer, they spend on average one third of their lives in post menopause. Unfortunately, this means their lives are impacted by a number of conditions related to their altered hormone levels, including osteoporosis. The benefits of the use of oestradiol and androgen subdermic implants have been demonstrated in publications resulting from studies and the results converge towards an improvement of the lipid profile and increase in the bone mineral density in the patients in post menopause.
Due to the increase in the number of women who survive on average one-third of their lives after menopause, osteoporosis, worsening of the lipid profile, and hypoandrogenic symptoms have become conditions of high cost to society1.
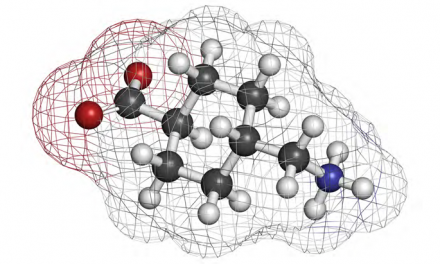
A physiological decrease in circulating levels of sex hormone-binding globulin (SHBG) occurs near menopause, together with an increase in the activity of the aromatase enzyme in certain tissues in order to encourage tissue-specific oestrogen production through androgenic precursors. This mechanism is the principal pathway of oestrogen production in menopause. Therefore, the most physiological manner in which to replace oestrogens and androgens in postmenopause is to increase the bioavailability of the endogenous androgenic precursors, a preferable alternative to providing exogenous oestrogens. Only 2% of testosterone, the free fraction not bound to SHBG, exerts a biological role on tissue, and oral oestrogen therapy increases the production of SHBG, diminishing the effects of endogenous testosterone and accelerating the appearance of symptoms of androgen deficiency2.
Nevertheless, the increase in SHBG levels is less evident when oestrogen therapy is administered in the form of subcutaneous implants, permitting testosterone to exert its effects on tissues. This is the rationale behind the use of oestradiol and testosterone in the form of subcutaneous implants for the relief of menopausal symptoms2.
Subdermal implants
The subdermal implants are fabricated in the institution using segments of surgical-grade, semipermeable Silastic® tubing (Technical Products, Inc., Decatur, GA, USA), steam-sterilised in an autoclave at 121 °C for 10 minutes and allowed to dry inside the autoclave for a further 10 minutes. Implants are submitted to microbiological and endotoxin control. The oestradiol implants, measuring 5 cm in length and 2.4 mm in external diameter, are filled with 50 mg of 17-beta-oestradiol, providing a release rate that ranges from 4 to 5 mg oestradiol/day over 1 year. A set of four implants of oestradiol annually releases, proportionally, a dose equivalent to that achieved with transdermal patches (50 mg/week), which is considered low-dose.
Testosterone implants measure 4 cm in length and 2.4 mm in external diameter, and are filled with 50 mg of 17-beta-testosterone, equivalent to a mean daily release rate of 0.2–0.8 mg/day over 1 year.
The implants were inserted using surgical steel trocars in the upper, outer quadrant of the gluteal region of the patients following local anaesthesia with 2% procaine.
The most adequate dose of implants to be used for each individual patient is decided on the basis of her medical history and physical and laboratory examinations.
Side-effects and complications
Although doses of several types of medication have been standardised, in a patient on hormonal therapy, changes in dose may be a result of various factors, including inadequate response and the appearance of minor, undesired side-effects such as mastalgia and cephalea. Individual factors may justify the use of higher doses of oestradiol in hormone therapy regimens, such as the concomitant use of some drugs, including smoking, that interact with this steroid and reduce its bioavailability. Implant site complications were reported by 3.6% of subjects during any of the assessments in clinical trials. Pain was the most frequent implant site complication, reported during and/or after insertion, occurring in 2.9% of subjects. Additionally, haematoma, redness, and swelling were reported by 0.1%, 0.3%, and 0.3% of patients, respectively.
Hormone therapy
During menopause, women may experience greater loss of bone mineral density (BMD), mainly in the first 3–4 years, leading to a high risk of fractures and their consequences for patients in this stage of life3. The relationship between postmenopause osteoporotic fractures and the decline of ovarian function was previously established. Oestradiol has great importance in the maintenance of bone micro-architecture, and transdermal forms have high effectiveness in preventing osteoporosis and fractures4–6.
Women in menacme have a natural protection against cardiovascular diseases. Until the middle of the last decade, hormone therapy was indicated for cardiovascular protection and many observational studies showed a betterment in the lipid profile and reduction in the cardiovascular risk among users of hormonal therapy. Some studies show menopause worsens women’s lipid profiles, the use of oestradiol combined with progesterone has shown worsening of the lipid profile with increase of low-density lipoprotein (LDL)-cholesterol and cardiovascular risk7–12. The behaviour of the lipid profile in women using the combination of oestradiol and testosterone is not well defined and the results of the studies are overly controversial13–15. A number of studies have presented a reduction of total cholesterol (TC)13–15 when using this combination. However, a reduction in high-density lipoprotein (HDL) levels was also witnessed.
In a study by Castelo-Branco et al16, androgen therapy was associated with significant increases in total cholesterol, LDL, and triglycerides (TG). The study recruited 120 patients from Barcelona, Spain. Using estradiol valerate 4 mg and 200 mg of intramuscular enanthate of dihydroandrosterone every month, after 1 year they found an increase of 16.9% in TC, 8% in LDL, 6.5% in TG, and reduction of 2.7% in high-density lipoprotein (HDL).
Benefits to bone density
The benefits of hormonal therapy were demonstrated in recent studies through the increase of bone mineral density among users of a oestradiol plus testosterone combination. The use of testosterone seems to further increase the bone mineral density in relation to the isolated use of oestradiol17,18.
Britto et al, studied 61 Brazilian patients in prospective cohort study using implants of oestradiol and testosterone. BMD assessment through dual energy X-ray absorptiometry showed addition of 1.87% in the lumbar spine and 3.8% in the femur neck BMD in women using implants, and a decrease in BMD lumbar of 5.92%, and 5.06% in the femur neck, without implants, after 1 year19.
In a study taken in London with 364 women in post menopause, Garnett et al showed a difference in the digital radiography of 1123 grams of hydroxyapatite (gHa)/cm2 in the group treated with 75 mg of oestradiol and 100 mg of endodermic testosterone versus 0.951 gHa/cm2 in the control group17.
Studd et al studied 213 patients using oestradiol implants (75 mg) and testosterone (100 mg) and showed an increase of 8.3% and 2.8% in bone density and lumbar spine and femoral neck after 1 year18.
Davis et al showed the use of testosterone improved the effects of oestradiol on bone density in a prospective 2 year study of with 34 Australian women in post menopause using implants of 50 mg of oestradiol or oestradiol plus testosterone (50 mg). A bone densitometry (DEXA) was carried out and found an increase of 10% and 8.8% in bone density in the femur and lumbar spine (L1–L4) in the group using oestradiol plus testosterone, compared to 2.4% and 3.5% in the group using isolated oestradiol20. The favourable oestrogenic effects on lipids were preserved in women treated with testosterone, in association with beneficial changes in body composition.
Savvas et al studied 20 women from London, UK, who were using long-term oral oestrogen in post-menopause, and inserted implants of oestradiol plus testosterone in 10 patients. They observed an increase of 5.7% of bone density in lumbar spine and 5.2% in femoral neck in these women, through the bone mineral densitometry (DEXA) after 1 year. In women who kept using oral isolated oestradiol there were no changes in bone density21.
Lipid profile
Britto et al studied 122 patients in a 1 year prospective cohort using implants of oestradiol and testosterone and observed improvement in the lipid profile (total cholesterol, HDL and triglycerides) after 1 year22.
Farish et al studied 14 oophorectomized women treated with 50 mg implants of oestradiol and 17 with implants of oestradiol plus testosterone (50 and 100 mg respectively). During 6 months they showed that the LDL reduced in both groups and LDL did not suffer modifications in the group taking oestradiol plus testosterone23.
One benefit of the use of implants is the continuous maintenance of serum levels of oestradiol and testosterone. Filho et al, studied 258 women using oestradiol and testosterone implants resulting in blood levels that ranged from 35 to 50 pg/mL of oestradiol and physiological blood levels that ranged from 50 to 80 ng/dl of testosterone. Zang et al, studied 63 women using oral testosterone undecanoate 40 mg and oestradiol valerate (2 mg daily) and found an average of 40–49 ng/dl of serum testosterone24,13, which is within average levels for females.
Conclusion
The benefits of the use of oestradiol and androgen subdermic implants have been demonstrated in publications resulting from studies with a reduced number of patients, in non-probabilistic samples, and most of them observational. On the other hand, the results converge towards an improvement of the lipid profile and increase in the bone mineral density in the patients in post menopause. Additional studies are being conducted by the author to further support the use of subdermic implants for hormone replacement therapy.