Mukta Sachdev, MD, and Ninon Patrao, MD, take a comprehensive look at the diagnosis and treatment options available for hyperpigmentation in skin of colour
Skin of colour represents the non-Caucasian darker shades of skin ranging from black, brown, olive, and tan. It comprises the skin of ethnic descent typically spanning the Asian, African, Mediterranean, Middle-Eastern, Hispanic and Native American racial backgrounds.
There are a number of classifications based on genetic disposition, reaction to sun exposure and cosmetic interventions, and the tanning properties of the skin, these include Fitzpatrick, Robert’s, Obagi, Kawada, and Glogau.
Lately, a new genetico-racial skin classification has been introduced by Fanous et al., which highlights the importance of incorporating the genetic and racial origin of the patient during assessment. The ‘north-to-south’ phenomenon that depicts the change in skin colour and features across the globe forms the base for this classification. The important variables that have been taken into account are the colour of the skin, thickness of the skin, and facial characteristics. Accordingly, six genetico-racial subtypes are described from the three founding races1.
What is responsible for skin colour?
Melanin
Colour in humans is determined by a group of complex pigments called melanin, which is responsible for the colour imparted to skin hair and eyes.
Chemically, melanins may be classified broadly into eumelanin (eu = good) and pheomelanin (pheo = cloudy or dusky). Eumelanin is prevalent in individuals with black and brown hair and pheomelanin is responsible for red hair and freckles. Studies have shown that darker skin has higher total melanin and eumelanin content, and a higher ratio of eumelanin to pheomelanin than those derived from lighter skin4.
Melanocyte
Melanocytes synthesize melanin in a special organelle called melanosome and move along arm-like structures named dendrites of the melanocyte to be transferred to epidermal keratinocytes. In humans, each melanocyte transfers melanosomes to around 30 surrounding keratinocytes, forming the melano-epidermic unit2.
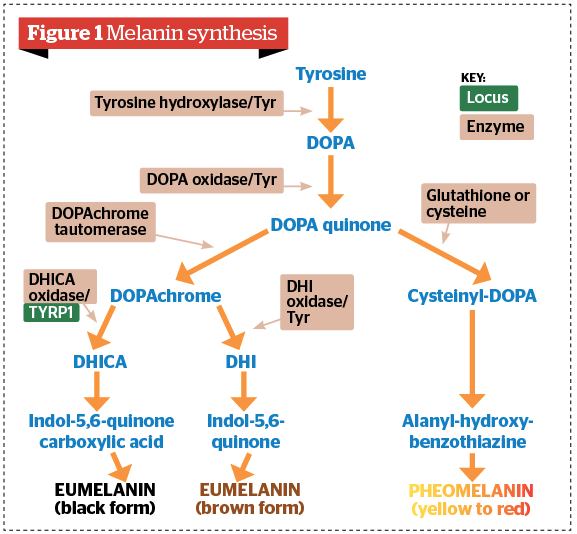
Melanin synthesis
Tyrosine is the common precursor for both eumelanin and pheomelanin production. The synthesis of melanin takes place inside melanosomes, following transfer of the enzyme tyrosinase, which oxidizes tyrosine to dihydroxyphenylalanine (DOPA) and dopaquinone (DQ). Large bioaggregates composed of homo or hetero-units of pheo and eumelanin compounds are formed by oxidation and cyclization of the initial substrate, tyrosine7.
The hyperpigmentation quandary
Human skin contains a mixture of melanin types, the ratio which, in part, determines visible pigmentation. The diversity of skin pigmentation among different ethnic groups is preserved and depends on eumelanin content. The ratio of eumelanin to total melanin is what decides skin colour. Pheomelanin does not correlate with skin pigmentation as a similar amount of this pigment is observed in dark as well as light skin8.
Being the most potent blocker of ultraviolet radiation (UVR), the role of melanin in photo-protection is complex. This is because one type of melanin, called eumelanin, is UV absorbent with a higher resistance to degradation and has the ability to neutralize reactive oxygen species; whereas the other, pheomelanin, is photo-unstable10.
Skin hyperpigmentation may be caused by stress or exposure to sunlight, which stimulates the release of α-melanocyte stimulating hormone (α-MSH) from damaged keratinocytes. The receptor (MC1R) acts as a signaling molecule on melanocytes that responds to α-MSH by inducing an expression of enzymes responsible for eumelanin (brown/black melanin) synthesis10.
Conditions causing facial hyperpigmentation in skin of colour
They may be categorized as follows:
- Diffuse:
- Melasma
- Exogenous ochronosis
- Riehl’s melanosis
- Lichen planus pigmentosus
- Localized:
- Periorbital melanoses
- Nevus of Ota
- Lesional:
- Dermatosis papulosa nigra
- Metabolic:
- Addison’s disease
- Haemochromatosis
- Neck-involved hyperpigmentation:
- Acanthosis nigricans
- Erythema dyschromicum perstans
- Poikiloderma of civatte
- Post-inflammatory
- Drug-induced
- Rare:
- Erythromelanosis follicularis faciei et colli
- Erythromelanosis peribuccale pigmentaire of brocq
- Argyria
- Post-chikungunya pigmentation.
Some of the conditions encountered in clinical practice have been discussed briefly below.
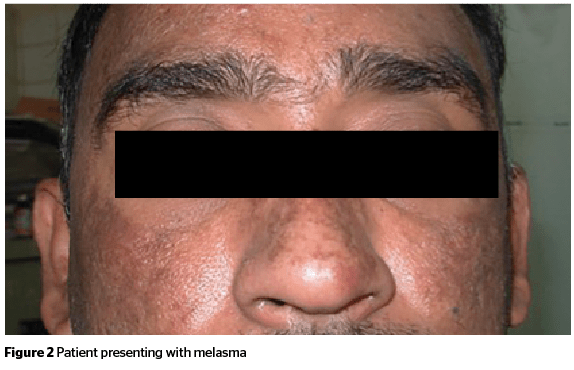
Melasma
Melasma is an acquired symmetric hypermelanosis most commonly visible over the face.
Aetiology
Melas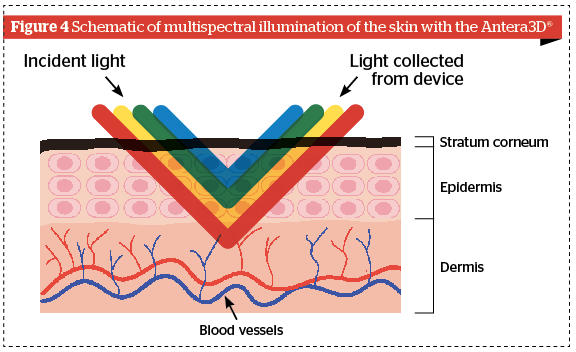
Melasma is known to have a multifactorial aetiology. Contributing factors include increased UV exposure, pregnancy, cosmetics, genetic factors, endocrine factors, and hormonal therapy13.
Clinical aspects
It is characterized by development of slowly enlarging tan-brown macules and patches. The most common sites of involvement over the face are the cheeks, forehead, upper lip, nose and chin (sun-exposed areas)14.
Types
On the face, three patterns of melasma are recognized:
-
-
- Centrofacial: pigmentation on cheeks, forehead, upper-lip, nose, and chin
- Malar: pigmentation present only on cheeks and nose
- Mandibular: pigmentation on ramus of the mandible.
- Depending on the natural history of the lesions, melasma may also be classified into:
- Transient type: which disappears within a year of withdrawal of hormonal stimulus
- Persistent type: which persists for more than a year after withdrawal of hormonal stimulus and is maintained by UVR and other factors.
- Based on visible light, Wood’s light examination, and skin histology (the location of melanin), melasma is classified into:
- Epidermal: in which the pigment is brown and margins of the lesions are well defined and geographical
- Dermal: in which the pigment is grey-brown and the margins of the lesions are poorly defined
- Mixed or epidermo-dermal: in which melanin is present both in the epidermis and dermis
- Indeterminate: in which it is difficult to classify melasma, even with Wood’s light15.
-
Exogenous ochronosis
It is a cutaneous disorder characterized by blue-black pigmentation mainly on the photo-exposed areas.
Aetiology
It occurs when foreign substances cause homogentisic acid to be deposited in the dermis, causing macular and papular hyperpigmentation. It commonly results from the use of topical hydroquinones but has also been associated with the use of phenol, quinine injection, resorcinol, picric acid, mercury, and oral antimalarials16.
Clinical aspects
It presents as asymptomatic bilaterally symmetrical speckled blue-black macules and several grey-brown macules, typically affecting the malar areas, temples, lower cheeks, and neck16.
Riehl’s melanosis
Riehl’s melanosis also referred to as pigmented contact dermatitis, is characterized by a brown-grey colour over sites of application of contactants, especially cosmetics17.
Aetiology
Cosmetic allergens include red and yellow pigments, chromium hydroxide, aniline and azo dyes, bactericidal agents (carbanilide, ricinoleic acids), hair dyes, red kumkum15, and fragrances. Textile allergens include optical whiteners, dyes, textile finishes, mercury compounds, formaldehyde, and rubber components18.
Clinical aspects
Lichen planus pigmentosus
Is a condition characterized by persistent and asymptomatic slaty-grey pigmentation, predominantly on the face.
Aetiology
Lichen planus pigmentosus (LPP) is a disease of the middle-aged, with onset in the third to fourth decades of life with female preponderance. It is a variant of lichen planus that favours skin phototypes III–V and has been known to occur more in tropical areas. Incriminating agents include cosmetics, such as fragrances, hair dyes, mustard oil, and amla oil20.
Clinical aspects
LPP manifests as pigmentation of insidious onset without any features of inflammation or preceding raised lesions.
It presents as oval or irregularly shaped slaty-grey to brownish-black pigmented macules and patches in sun-exposed areas, including the forehead, temples, and neck, or intertriginous areas.
It is typically asymptomatic, although, occasionally can have mild pruritus. The course is variable with some cases showing spontaneous resolution within weeks to months. It may also be persistent over the years in many21.
Periorbital hyperpigmentation
Periorbital hyperpigmentation (POH) is characterized by light- to dark-coloured, brownish-black pigmentation surrounding the eyelids.
It is a commonly encountered condition and also referred to as idiopathic cutaneous hyperchromia of the orbital region (ICHOR), periorbital melanosis, dark circles or infraorbital pigmentation22.
Aetiology
It is known to have primary or secondary aetiology. The cause of secondary periorbital hyperpigmentation often has a multifactorial pathogenesis, including genetic or constitutional pigmentation, dermal melanocytosis, post‑inflammatory hyperpigmentation secondary to atopic dermatitis, allergic contact dermatitis, periorbital oedema, and excessive subcutaneous vascularity and shadowing due to skin laxity associated with ageing. Excessive sun exposure, drugs, hormonal causes, and an extension of pigmentary demarcation lines have also been considered to be contributory23.
Clinical aspects
It is an ill-defined entity that presents as bilateral round or semicircular homogenous brown or dark brown pigmented macules in the periocular region24.
Nevus of Ota
It is a dermal nevus characterized by bluish pigmentation in the distribution of the first and the second division of the trigeminal nerve25.
Aetiology
It occurs predominantly in more darkly pigmented individuals, especially in Asian and African-American people. The lesions occur during infancy, with the majority presenting at birth, and also around puberty26.
Clinical aspects
It is characterized by a blue-grey confluence of individual macules varying from pinhead-sized to several millimetres in diameter. The most common sites of involvement are the periorbital area, temple, forehead, malar area, earlobe, pre- and retroauricular regions, nose and conjunctivae with involvement of the ipsilateral sclera being a typical feature26.
Dermatosis papulosa nigra
A condition where benign epithelial tumours develop on the skin.
Aetiology
They are more commonly seen in darker-skinned persons, including those of African descent, Hispanics, and Asians. They have a familial tendency and become more frequent with advancing age27.
Clinical aspects
Multiple, small, 1–5 mm diameter, smooth, firm, black or dark brown papules on cheeks, forehead, neck, upper back, and chest28.
Acanthosis nigricans
It is a dermatosis characterized by thickened, hyperpigmented plaques, typically on the intertriginous surfaces and neck.
Aetiology
It is commonly associated with insulin resistance and obesity and, hence, early diagnosis of conditions, such as type 2 diabetes, the metabolic syndrome, and polycystic ovary syndrome is important. It is much more common in people with darker skin pigmentation especially Latinos and African Americans29.
Clinical aspects
It is characterized by dark, coarse and thickened skin with a velvety texture, being symmetrically distributed on the neck, the axillae, antecubital and popliteal fossae, and groin fold30.
Erythema dyschromicum perstans
Also known as Ashy dermatosis, it is a disorder of pigmentation, characterized by asymptomatic symmetric ashy grey-coloured macules.
Aetiology
It usually presents during the second to third decade of life and appears to be more common in areas of Latin America and Asia. There is no genetic predisposition, and it affects both genders equally. Ingestion of ammonium nitrate, ethambutol, radio-contrast media or chlorothalonil, nematode infestation, and occupational allergy to cobalt have been implicated invariably but its aetiology remains obscure31.
Clinical aspects
It presents as slate-grey to blue-brown oval, circular or irregularly shaped macules and patches that gradually develop into a symmetric distribution. Lesions typically involve the trunk with spread to the neck, upper extremities, and the face32.
Poikiloderma of civatte
It is a skin condition characterized by erythematous and brownish patches seen mainly on the sides of the neck and peripheral face.
Aetiology
The condition is most common in fair-skinned individuals in the fourth to seventh decade. There is a female predominance. Predisposing factors include exposure to solar radiation, photosensitizing chemicals in cosmetics and perfumes, hormonal changes related to menopause or a low oestrogen state, and genetic susceptibility33.
Clinical aspects
It presents with a combination of linear telangiectasia, erythema, mottled hyperpigmentation, and superficial atrophy in a reticular pattern, symmetrically affecting the sun-exposed areas, such as the sides of the neck, lateral cheeks, and upper chest. The shaded area under the chin is characteristically spared34.
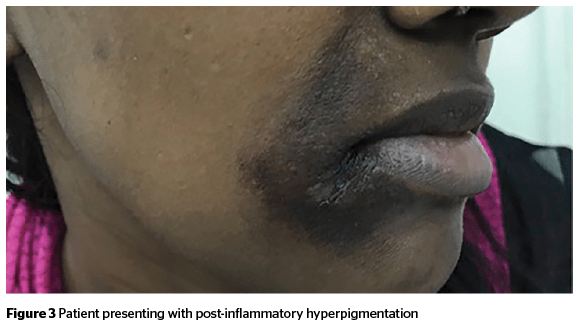
Post-inflammatory hyperpigmentation
Post-inflammatory hyperpigmentation (PIH) is an acquired hypermelanosis occurring after cutaneous inflammation or injury that can arise in all skin types, but more frequently affects skin-of-colour.
Aetiology
A wide range of aetiologies for PIH exists, including infections, such as dermatophytoses or viral exanthems; allergic reactions, such as those from insect bites or a contact dermatitis; papulosquamous diseases like psoriasis or lichen planus; medication-induced PIH from hypersensitivity reactions; or cutaneous injury from irritants, burns, or cosmetic procedures. The hyperpigmentation results from the melanocytes’ response to the cutaneous insult, which causes an increased production and/or redistribution of melanin35.
Clinical aspects
PIH typically manifests as macules or patches in the same distribution as the initial inflammatory process. The time required for the dyspigmentation to normalize is highly variable and relates to many factors, including the patient’s baseline skin tone, the type and intensity of the injury or inflammation, and the patient’s sun-exposure habits36.
Drug-induced hyperpigmentation
Drug-induced pigmentation represents 10 to 20% of all cases of acquired hyperpigmentation.
The main drugs implicated in causing skin pigmentation are:
-
-
- Antimalarials
- Tetracyclines
- Minocycline
- Oral contraceptives
- Amiodarone
- Cytotoxic drugs
- Clofazimine
- Chlorohexidine
-
The pathogenesis of drug-induced pigmentation is variable according to the causative medication and can involve an accumulation of melanin, sometimes following a non-specific cutaneous inflammation and often made worse by sun exposure, an accumulation of the triggering drug itself, a synthesis of special pigments under the direct influence of the drug or deposits of iron following damage to the dermal vessels37.
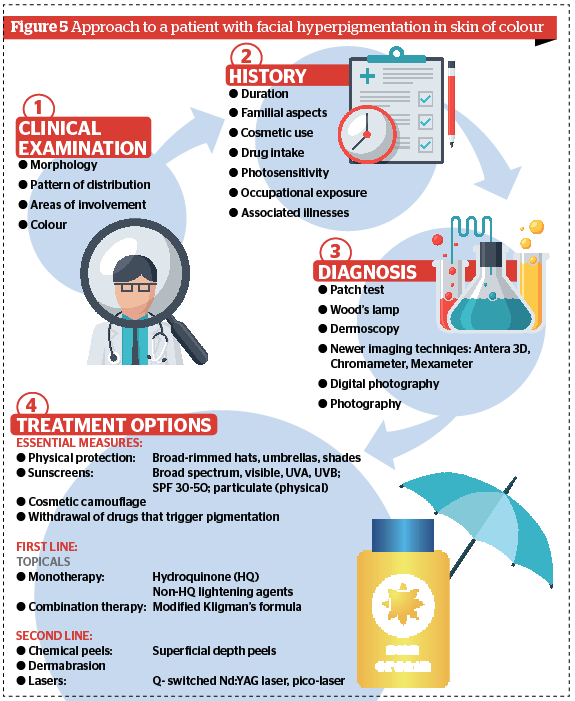
Diagnosis
Patch test
Increasing use of cosmetics has contributed to a rise in the incidence of allergic contact dermatitis (ACD). It is estimated that 1–5.4% of the population is sensitized to a cosmetic ingredient. Patch testing helps to confirm the presence of an allergy and to identify the actual allergens, which are chemical mixtures of various ingredients38.
Wood’s lamp
Wood’s lamp can be used to determine the depth of melanin in the skin. The variations in epidermal pigmentation become more apparent under Wood’s light, such as in brown hypermelanosis or epidermal melasma. For dermal pigmentation, this contrast is less pronounced, as with dermal melasma.
Dermoscopy
Dermoscopy is an in vivo method for the diagnosis of pigmented lesions of the skin. Light is either reflected, dispersed, or absorbed by the stratum corneum because of its refraction index and its optical density, which is different from air. Thus, deeper underlying structures cannot be adequately visualized. However, when various immersion liquids are used, they render the skin surface translucent and reduce the reflection, so that underlying structures are readily visible. The application of a glass plate flattens the skin surface and provides an even surface. Optical magnification is used for examination. Taken together, these optical means allow the visualization of certain epidermal, dermo-epidermal, and dermal structures39,40.
Antera 3D® imaging
Antera 3D® relies on multidirectional illumination obtained by LEDs of different wavelengths from different directions followed by a computer-aided reconstruction of the skin surface and using the differences between these images to reconstruct the surface in three dimensions. The skin topography and the chromophores’ concentration are derived from the spatial and spectral analysis of the acquired image data. The acquired spectral data is used to map the distribution and concentration of melanin and haemoglobin (Figure 4).
Unlike traditional imaging techniques, where only three colour channels (red, green, and blue) are used, the Antera 3D® uses reflectance mapping of seven different light wavelengths spanning the entire visible spectrum. This allows for a much more precise analysis of the skin colourimetric properties, which are mostly determined by two dominant chromophores: melanin and haemoglobin. The qualitative evaluation of various aesthetic dermatologic conditions using this technique appears promising.
Tristimulus colourimetry
The principle behind this instrument lies in the fact that it is analogous to the way our eye perceives colour. It uses white light to illuminate the skin and then measures the intensity of the reflected light through three filters of particular wavelength or photodiode arrays42.
The most commonly used tristimulus colourimeter instrument is the chroma meter.
Chromo meter
The Chroma Meter® CR-400 (Konica Minolta, Tokyo, Japan) device measures the intensity of reflected light and the colour of the skin surface through filters of 450, 560, and 600 nm wavelengths. The skin surface is illuminated with polychromatic light (pulsed xenon arc lamp) and the signal from the skin is reflected into the device and separated into its spectral components using the L*a*b* system of the Commission Internationale de l’Eclairage (CIELab). Briefly, the components are L* for luminance/brightness, the higher the value, the higher the intensity; a* for red/green components of light, positive values representing the red component and negative values representing the green component; and b* for yellow/blue components of light, positive values representing the yellow component of the light and negative values representing the blue component43.
Narrowband spectrometers
They consist of light-emitting diodes to illuminate the skin surface and the intensity of reflected light is recorded using a photodetector.
The most widely used narrowband spectrophotometers are:
-
-
- DermaSpectrometer (Cortex Technology, Hadsund, Denmark)
- Erythema/Melanin Meter (DiaStron, DiaStron Ltd., Hampshire, UK)
- Mexameter M X16 (Courage Khazaka).
-
The benefit of these instruments is that they can distinguish between two main pigments of the skin, such as melanin and haemoglobin, using their distinct spectral curves44.
DermaSpectrometer uses two light emitting diodes, green (568 nm) and red (655 nm) to illuminate the skin and the amount of the reflected light is measured using a photodetector.
Mexameter uses 16 light-emitting diodes that emit light at three wavelengths — green (568 nm), red (660 nm), and infrared (880 nm). Results are expressed in terms of ‘melanin index (MI)’, a quantitative measurement of melanin, and ‘erythrema index (E)’, a quantitative measurement of skin redness45.
Treatment
Facial hyperpigmentation causes a lot of cosmetic concern in patients with a tremendous emotional impact. Treatment is essentially focused on removal of provoking factors, photoprotection, and some form of active pigment reduction either with topical agents or physical modes of treatment. There is no universally effective specific therapy and existing agents possess varying degrees of efficacy with relapses being frequent.
Essential
Photo-protective measures
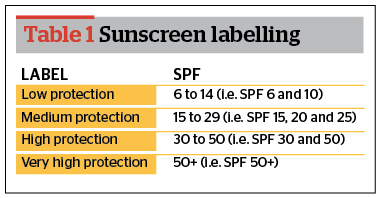
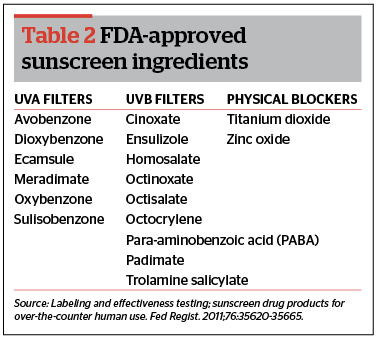
Sunscreens
Broad-spectrum UVA and UVB protective sunscreen with an SPF of at least 30 including a physical block (e.g. titanium dioxide or zinc oxide) should be used for prevention of facial hyperpigmentation.
Individuals with darker skin tones who tan easily and rarely burn may feel they do not need to use sunscreen. However, like sunburn, a tan is the result of DNA damage from exposure to the sun’s harmful UV radiation. Darker-skinned people may also be wary of using physical sunscreens, especially titanium-based products because they can look chalky and white on the skin. Newer preparations, however, tend to be micronized, which means the particles are small enough to allow them to blend in and disappear into the skin. Chemical sunscreens are also an option; look for a broad-spectrum sunscreen with an SPF of 15+46.
Cosmetic camouflage
Sunscreens containing zinc oxide, 10% and SPF of 30 have dual benefit of camouflaging hyperpigmentation over the face and preventing photo-induced darkening36.
First-line
Skin lightening agents
Hydroquinone
It is an hydroxyphenolic chemical that has been the gold standard for treatment of hyperpigmentation for many years.
The efficacy of hydroquinone (HQ) in facial melanoses (FM) depends on several factors. Epidermal pigmentation responds better than dermal. Higher concentrations give better results (4% being more effective than 2%) as their onset of action is earlier than those with lower concentrations. Antioxidants, such as vitamin C and retinoids, as well as alpha-hydroxy acids, may be used as additives to increase penetration and enhance efficacy47.
Adverse reactions to hydroquinone are dose and duration dependent. Reactions include asymptomatic transient erythema, irritation, confetti-like depigmentation with higher concentrations and exogenous ochronosis48.
Azelaic acid
Azelaic acid is well tolerated with the most commonly reported side-effects including pruritus, mild erythema, scaling, and burning50.
Kojic acid
It acts by chelating the free portion (copper) of tyrosinase. This is brought about by reducing o-phenones to diphenols. In addition, it has antioxidant and photoprotective properties. It is stable and used in concentrations of 1–4%51. It is generally preferred as a second line therapy due to its good safety profile and stability especially when other therapies are not tolerated. It can be used along with other topical medications as well as peels. Adverse effects include contact dermatitis, irritation and erythema52.
Arbutin
This natural plant product acts by inhibiting tyrosinase and decreasing melanin formation. The hydrolyzed product of arbutin acts as a free-radical scavenger and is more effective in inhibiting tyrosinase than arbutin. Its action is dose-dependent and has less severe adverse effects than HQ. Recently, a derivative of arbutin, namely deoxyarbutin, has been developed by removing hydroxyl groups. It produces reversible skin lightening by directly inhibiting tyrosinase53.
Retinoids
Retinoids (retinoic acid, tretinoin, adapalene, tazarotene) have been used to treat melasma and PIH, either as monotherapy or combined with other agents including hydroquinone and topical steroids54.
Used as monotherapy, 0.1% RA is more effective than 0.05% and 0.025%, but is also more irritating. With isotretinoin the response is equivocal but in Indian patients, adapalene is as efficacious as RA but with significantly less irritation. Though RA takes longer than HQ to act, the response when combined with HQ (5%), and lactic acid (7%) or ascorbic acid (10%) is not only more effective but faster as well. Irritation is the most common side-effect and may even cause hyperpigmentation; although, it is more frequent with higher concentrations of RA and less with adapalene. Photosensitivity is also common55.
Ascorbic acid
Ascorbic acid, also known as vitamin C, has been used in a variety of cosmetic preparations as an antioxidant, pH adjuster, anti-ageing and photoprotecting agent. Since it is unstable in aqueous solution, esters with similar properties are used. It can be used alone or in combination therapy. But this molecule is rapidly oxidized, highly unstable and does not work well alone; it is, therefore, usually combined with other agents such as liquorice extracts and soy to increase efficacy. It has a good safety profile56.
Niacinamide
It is an important component of many over-the-counter lightening creams. It reduces pigmentation by reversibly preventing transfer of melanosomes from melanocytes to the keratinocytes without affecting the tyrosinase activity57.
Glycolic acid
Glycolic acid acts in hyperpigmentation probably due to its effect on epidermal remodelling and accelerated desquamation. Side-effects include irritation and erythema, which resolves upon withdrawal and moisturization58.
Newer agents
Tranexamic acid
N-acetylglucosamine
NAG has been shown to decrease melanin synthesis and downregulate the expression of various pigmentation-related genes. Clinical studies have used either NAG alone or in combination with niacinamide. Overall, NAG has high tolerance, ease of formulation and stability in solution making it a suitable depigmenting agent60.
Mequinol
Mequinol is a derivative of HQ. It acts as a competitive inhibitor reducing formation of melanin precursors. It is available as 2% solution containing 0.01% retinoic acid. Side-effects include irritation, halo-hypopigmentation, and depigmentation61.
Liquorice extracts
Liquorice is a root of the perennial herb. Glabridin and other oil-soluble derivatives of liquorice inhibit tyrosinase. Liquiritin, another derivative, reduces skin pigmentation, but without inhibiting tyrosinase. A 20% liquiritin cream was found effective at 4 weeks in treatment of melasma62.
Soy
Soybean trypsin inhibitor reversibly inhibits the protease-activated receptor-2 pathway that is needed for melanosome transfer. Inhibition of this pathway caused a dose-dependent loss of pigmentation by as early as 4 weeks at the highest tested dose63.
SMA-432
It is a prostaglandin E2 inhibitor and is known to have skin brightening properties64.
Methimazole
Methimazole is an oral antithyroid drug which has been recently discovered to have a depigmenting effect if used topically in a 5% preparation65.
4-n butylresorcinol
It is similar to hydroquinone and is a tyrosinase inhibitor.It is an effective treatment option for topical hyperpigmentation management66.
Flavonoids
They are natural polyphenolic chemicals with anti-inflammatory, antiviral, antioxidant and anticancer properties. Catechins with gallic acid, ellagic acid and aloesin are a few such compounds. Ellagic acid is an antioxidant derived from certain plants like eucalyptus, green tea, and strawberry. It suppresses melanogenesis by blocking tyrosinase and does not cause any damage to the cells67.
Lumixyl
It is a new oligosynthetic peptide that inhibits tyrosine. Containing 0.01% oligopeptide cream, 20% glycolic acid lotion, an antioxidant cleanser and physical sunscreen, it is found to accelerate clearance in mild to moderate melasma. A study revealed improvement in facial melasma and clearance in just 6 weeks68.
Beta-carotene
It is a structural analogue of vitamin A, which acts as an agonist to vitamin A, saturates melanocyte receptors, and reduces melanin production. It requires a prolonged duration of treatment but has few side-effects69.
Dioic acid

Antisense oligonucleotides
They act against tyrosinase, TRP-1 and TRP-2 at the molecular level by interacting with translation of targeted mRNA69.
Lignin peroxidase
Lignin peroxidase is a novel method of skin lightening and acts by targeting, enzymatically oxidizing and breaking down melanin in the skin. The application of lignin peroxidase cream provided a significantly more rapid and observable skin-lightening effect than 2% hydroquinone or placebo. Overall, lignin peroxidase is well tolerated with minimal to no side-effects71.
Miscellaneous
Mulberry extract, thiotic acid, phenolic-thioether, cinnamic acid, pidobenzone, silymarin, 4-isopropyl-catechol and linoleic acid with lincomycin69.
Combination therapy
Topical agents act on different stages of melanogenesis; therefore, when combined, give better therapeutic results. Agents are also combined to reduce untoward effects, such as topical steroids reduce irritation due to both HQ and retinoids and retinoids themselves counter steroid-induced atrophy. Some agents are used as ‘stabilizers’ and hypomelanotic agents are often combined with sunscreens. HQ is the most commonly used agent, often being combined with glycolic acid, azelaic acid, kojic acid and retinoic acid, or corticosteroids.
The most extensively studied and widely used combination with HQ is with RA and corticosteroids; this ‘triple combination’ is also called Kligman’s formula. Its original combination contained 5% HQ, 0.1% tretinoin, and 0.1% dexamethasone. Due to irritation, the combination has been modified to reduce HQ to 2−4% and tretinoin to 0.025−0.05% and the steroid has been variously changed to fluocinolone acetonide or others. It is extensively used as first-line therapy for melasma and other FM34.
Second line
Chemical peels
Chemical peels are generally effective in darker skin, especially superficial peels. Due to the increased risk of PIH, deep peels should be avoided. Pretreatment with a course of hydroquinone may improve results. Topical retinoids should be stopped before seven days.
Standard options are glycolic acid 10–70%, salicylic acid 20–30%, trichloroacetic acid (TCA) 10–25%, and Jessner’s solution. Newer options include tretinoin, pyruvic acid, β-lipo hydroxy acid, mandelic acid, and amino fruit acids72.
When selecting a peeling agent, the benefits of the procedure should always substantially outweigh any associated risks or complications. Superficial peels with appropriate titration of concentrations are generally safe and efficacious for darker skinned patients.
Clinicians should be acutely aware that deeper peels carry substantial risks of inducing scarring and hypopigmentation in darker skinned racial-ethnic groups73.
Lasers

Many reports have pointed out that the safest and most efficient laser for darker skin is the Q-switched Nd:YAG laser with its longer wavelength (1064 nm). A recent study has concluded that pulse-in-pulse IPL (PIP-IPL) might be a safe and promising treatment for melasma in darker skin. Fractional photothermolysis laser 1550 nm and fractional CO2 laser are also effective laser options75,76.
A new class of lasers that generate picosecond-domain pulses. Shorter laser pulse durations result in pigment fragmentation that is more a result of photoacoustic than photothermal effects. Therefore, it may be more efficient at pigment removal without inducing thermal damage to the surrounding tissue. Picosecond lasers are currently available with laser outputs of 532 nm, 755 nm, and 1064 nm. However, their efficacy is still to be established77.
Treatment with lasers for facial hyperpigmentation has been associated with an unpredictable response, frequent relapses and high risk of both post-inflammatory hyper- and hypopigmentation. Proper patient counselling in regards to side-effects and expectations along with test patch should always be employed prior to any laser procedure.
Dermabrasion
Patients with resistant melasma, especially with a prominent dermal component, have been successfully treated with local or full-face dermabrasion to the upper or mid dermis using a 16-mm diameter coarse grit diamond fraise. Side effects may include hypertrophic scars or permanent hypopigmentation but are extremely rare78.
Conclusion
Facial hyperpigmentation in skin of colour can be extremely distressing for a patient. There is a significant impact on the patient’s quality of life; therefore, an accurate diagnosis, effective treatment, and patient counselling is imperative. The physician’s judicious choice of procedure with flexible treatment strategy is important, and emphasis on the need for a long-term maintenance therapy needs to be advised.