Procedure
Before the procedure begins, a supraorbital nerve block is administered with local anaesthesia. The lid can then be everted over a Desmarres retractor. Next, the superior border of the tarsus is outlined with a marking pen (Figure 1), and the conjunctiva superior to the tarsus is gently pulled with forceps to separate the Müller muscle from underlying levator aponeurosis.
Calipers are used to measure the amount of tissue excision desired above the superior tarsus and this is marked on the conjunctiva; 8 mm is the usual length for full correction. A mullerectomy clamp is then placed to encompass the demarcated tissue consisting of Müller muscle and conjunctiva. Small haemostats can also be used if a clamp is unavailable.
A size 6-0 double armed plain suture is run along the underside of the clamp starting at the temporal edge (Figure 1e). When the medial edge has been reached, a number 15 blade (#15) is used to make an incision along the underside of the clamp, the clamp and its enclosed tissue can then be removed.
The suture can now be run from the medial to temporal, hooking the conjunctiva and Müller muscle to the superior edge of the tarsus. At the temporal edge, the two ends of the suture are passed through the wound so that the knot will be buried when the suture is tied.
Postoperatively
The patient is instructed to use ice compresses for the first 3 days. Starting on the fourth day, they will switch over to warm compresses. A combination of antibiotic and steroid drop or ointment can be used for the first week. The patient will usually have some mild oedema and bruising, as well as often have a foreign body sensation in the eye when they blink for the first 2–3 days since the incision is internal. Artificial tears will help to diminish this discomfort.
Complications
Complications from this ptosis repair can include over‑ and undercorrection. For an overcorrection, gentle massage should be carried out on the lid to help stretch the wound as it heals. If the lid does not lower sufficiently, it can be everted, and the wound can be opened at the superior border of the tarsus to recess the Müller muscle, and allowed to granulate in. The only real complication from overcorrection is exposure keratitis. This can be treated with lubricant drops, and if severe, the lid can be lowered surgically.
For an undercorrection, the patient should be followed for a number of months. While most patients will have a good lid position by 1 week, there are some patients whose lids do not elevate completely until 3–4 months postoperatively. If they are still low at 6 months, the surgery can be repeated.
Most patients will experience some dryness after surgery and should use lubricant drops and ointments based on the severity of their symptoms. Both over- and undercorrection are rare with this procedure.
Discussion
A Müller muscle–conjunctival resection is an excellent and popular technique for correction of involutional ptosis. An internal approach for ptosis correction was initially described by Fasanella and Servat in 196110. They everted the eyelid and resected a portion of the superior tarsus to advance the levator. In 1975, Putterman and Urist11,12 described an alternative internal approach with resection of Müller muscle and conjunctiva but preservation of the tarsus. In this surgery, the resection begins at the superior border of the tarsus and a segment of conjunctiva and Müller muscle are removed. Studies have shown that some levator aponeurotic fibres are incorporated into the resected tissue, which may play an important role in the eyelid elevation.
The amount of surgical resection can be based on the result of the preoperative phenylephrine test. The elevation seen with the test will correspond to the amount of correction attained with an 8 mm surgical resection. If a patient appears overcorrected with the phenylephrine, less than 8 mm of resection should be performed. If they have residual ptosis with the phenylephrine, between 9 mm and 10 mm of Müller muscle should be resected.
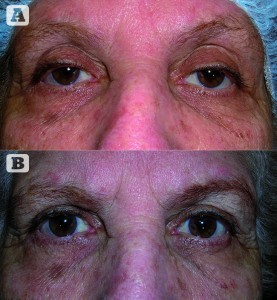
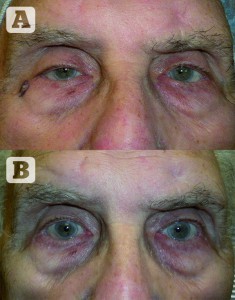
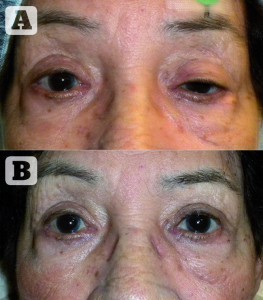
The results with this procedure are consistently excellent, and the postoperative lid height more predictable than with an external levator resection. Lid contour abnormalities are very rare with this procedure. Because of this it is becoming a more popular choice for surgeons who do ptosis surgery. It is also easily combined with an upper eyelid blepharoplasty, so that both the dermatochalasis and ptosis are repaired.
Conclusions
Müller muscle–conjunctival resection is an excellent technique for correction of involutional ptosis. It is a rapid procedure with minimal bleeding and recovery time. It can be combined with an upper eyelid blepharoplasty in patients with dermatochalasis. The outcomes of the surgery are very predictable, resulting in excellent lid height and contour, with high patient satisfaction and with similar results to the external levator resection for ptosis correction. The Müller muscle–conjunctival resection is becoming a more popular procedure and may become the standard procedure of choice in future.