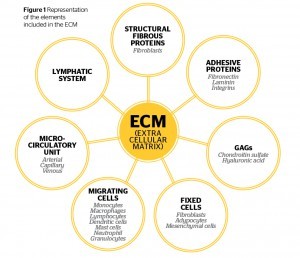
Cellulite (edematous fibro-sclerotic panniculopathy) or FEF (female evolutive fibroedema) represents an aesthetic pathology that requires a precise therapeutic strategy characterised by an integrated treatment with a variety methodologies. Cellulite is a very common condition in women in whom the skin acquires an orange peel or mattress appearance and is the result of a number of biochemical and metabolic changes. The presence of cellulite is a significant source of patient dissatisfaction. According to the most recent studies, those changes start in the ECM extracellular matrix. The physiopathology shows modification of the connective tissue and the extracellular matrix; a decrease in the microcirculatory (the network of diminutive arteries and veins) and lymphatic system, resulting in an interstitial oedema and microangiopathy due to stasis representing triggering factors that also support the pathological process. In the end hyperplasia and hypertrophy of the fat tissue with a sclera connective evolution occurred (skin retractions). The ECM is a three dimensional complex of proteins, carbohydrates, salts, fixed cells, migrating cells and fibres. An effective cellulite treatment should correct first the changes occurred in the extra cellular matrix, only way to achieve improvement in cellulite condition. The treatment of cellulite should follow different steps. The goal is to correct the physiopathology, all the changes produced in the ECM, connective tissue, microcirculation and adipose tissue.
Cellulite is certainly not a serious condition from the medical point of view but it does represent the most widely spread and least tolerated aesthetic complaint for women. The condition is well known due to intense publicity campaigns in the media as the cosmetics industry promotes its creams, electro-medical equipment, and pills. However, the importance of this purely aesthetic problem should not be underrated. Beauty plays an important role in human relationships in a social setting1.
Koblenzer2 mentions a number of studies that demonstrate real benefits from maintaining an appearance of youthfulness and beauty during all stages of life. When these patients stare in the mirror and see their cellulite, they experience diverse negative feelings, like anger, guilt, sadness, impotency, shame, discomfort, and the desire to cover themselves. Cellulite is an actual pathology, something uncomfortable and unaesthetic, which results in a disease for the patient. Our duty as physicians is to suggest the best scientific methods to repair tissue damage and pathological disorders.
Definition
There was a time when cellulite was conceived as a mere increase of fat in subcutaneous tissues associated with an altered lymphatic and venous flow and lymphatic stasis. Furthermore, there was a deeply-rooted notion that cellulite was closely related with the specific stasis subsequent to hypotonia or venous and lymphatic disease and it was assumed that a previous varicose disease should exist for cellulite to appear. In most cases, the interstitial alterations of cellulite appear first and the varicose or lymphatic pathology manifests itself only later. However, the characteristic orange peel appearance of cellulite is either due to an increase in the fat or interstitial liquid content, or to the alteration and retraction of connective layers occurring in different times and manners3.
Venous lymphatic stasis is the outward expression of malfunctioning in the endocrine-metabolic regulation of the interstitial matrix or extracellular matrix (ECM). Today we know that cellulite is the result of a number of biochemical and metabolic alterations that start on an interstitial matrix or ECM and connective structures level.
The ECM is represented by a complex structural entity that surrounds, nourishes, and furnishes support to all the cells. The main causes of alteration of the ECM are:
- Reduction of the arteriolar microcirculation
- Reduction of the cellular metabolism (increase free radicals)
- Increase the flogistic process at the connective tissue
- Alteration of the venous lymphatic system
- Lipodystrophy evolution.
Background
The term ‘cellulite’ was first used by Alquin and Pavot in France in 1920. Their insightful observations led them to associate this unaesthetic condition with a possible pathology accurately described a little later by Lagueze as a subcutaneous pathology characterised by ‘interstitial oedema associated with an increase in fat content’1.
In 1940, Allen described cellulite mainly as a typical lipoedema not accompanied by oedema in the foot. He further highlighted the prevalence of the metabolic alteration over venous-lymphatic impairment1.
In 1972, Braun and Falco made references to the predominantly vascular disease describing it as a lymphoedema with various manifestations.
Finally, in 1976, Reinharez, who had a deep knowledge of the lymphatic system, described this disease as an endocrine-metabolic pathology having secondary vascular and lymphatic manifestations1.
In 1978, Binazzi4, and later Sergio Curri5 — perhaps the greatest specialist on microcirculation together with Joseph Merlen — histologically proved the existence of microvascular alterations, dividing them into three groups: oedema, fibrosis, and sclerosis (hence the acronym EFP corresponding to oedematous fibrosclerotic panniculopathy).
Recent discoveries have led to different evaluations and, in 1997, Bacci et al described in Flebología hoy [Phlebology today] the conception of the cellulite disease as a ‘predominantly interstitial endocrine-metabolic pathology’1,6.
Today, we move our concept from Curri with the oedematous fibrosus panniculophathy to a new concept of Bacci: female evolutive fibroedema.
Female evolutive fibroedema
In the first instance, female evolutive fibroedema begins by initiating a functional alteration of ECM. Over time, there is a degenerative alteration of ECM with:
- Diminishing arteriolar microcirculation (<T˚)
- Increasing water in the fat tissue (lipoedema)
- Endocrine metabolic alterations (periphery mesenchimopathy)
- Decreasing venous lymphatic drainage (venous lymphatic oedema)
- Inflammatory and fibrosis in connective tissue and fat tissue
- Jellification of the ECM.
The final complications include:
- Surface hypoxia
- Lipodystrophy
- Tissular fibrosis
- Sclerotic connective evolution.
Observing the physiopathology of cellulite it is understandable why treatments should be integrated and not limited to just adipose tissue treatments.
What’s new in adipose tissue?
Adipose tissue (AT) has long been regarded as a resting tissue dedicated to energy storage and release. In recent years, this view has dramatically changed following new insights into the endocrine activity of adipocytes and the immunological functions of AT8. The biology of AT is a ‘black hole’ in the field of dermatology, aesthetic medicine, and aesthetic surgery, although the demand for surgical procedures involving the manipulation of subcutaneous AT is rising every year (surgical removal, liposuction, and lipofilling procedures). Physicians working in aesthetic medicine and cosmetic surgery taking out AT and placing it elsewhere with rather crude technology should think carefully about the fate of the tissue and cells they manipulate.
Predisposition to cellulite
There are many factors that have been shown to affect the development of cellulite and these include1:
- Family background, especially hereditary endocrine-metabolic syndromes, but also common nutritional deficiencies
- Body structure, especially postural and spinal column alterations
- Hormone imbalances in patients suffering from hormone functional alterations and patients consuming oestrogen or hormone-supplemented food
- Dietary disorders, particularly an excess of sugar, fat, and hormones
- Digestive disorders, especially those associated with intestinal flora alterations
- Disorders of the intestinal flora, which is the initial pathology in all degenerative tissue alterations such as arthrosis, myalgia, angiopathies, and cellulite pathologies
- Postural problems associated with foot orthopedic pathologies, such as inadequate footwear
- Psychosomatic disorders, especially depressive anxiety or languid, apathetic, and body dysmorphic disorder9
- Sexuality, a healthy balance between physiological and emotional needs ensures the chemical catalyst of many other metabolic functions. Lifestyle, poor diet, being obese or overweight, or having constipation are contributory factors
- External compression, tight clothing does not help the intestine lymph adipose system in its functions or the cutaneous microcirculatory system, thus favouring cellulite pathologies of the metabolic hypoxic type
- Infections may cause tissue damage, which, in turn, results in alterations and fibrosclerosis
- Smoking slows down microcirculation in the cutaneous arterioles and is thus lipogenetic, generating the cutaneous hypoxia traditionally known as orange peel skin. However, permanent and deceitful damages in the interstitium due to an excess of free radicals when defence mechanisms, such as superoxide dismutase (SOD), fail should also be assessed
- The intake of estro-progestagens, such as those included in birth-control pills and food preservatives. These favour interstitial liquid retention generating endothelial oedema and activating Fenton reactions. The process inevitably generates some form of lipoedema and lipolymphoedema, which in their turn result in lipodystrophy. Women who are administered hormones show a high level of free radicals as may be easily seen in Reactive Oxygen Metabolites (ROM) tests10,11.
Clinical evaluation of cellulite patients
As with other pathologies, the medical history should be detailed in the evaluation of cellulite. The patient should also be questioned regarding:
- The age of onset of cellulite
- Prior occurrence of trauma
- Liposuction or injections in the affected area
- The history of prior disease or surgery
- Family history
- The presence of chronic vascular or associated hormonal diseases
- The occasional or regular use of medications and previous or current history of hormonal treatment or the use of any medicine that may contribute to increase the deposit of fat in the affected areas
- Other aspects that should be researched with patients include if they are sedentary, diet programmes, psychosomatic factors, smoking habits, prior pregnancies, and the behavior of cellulite during pregnancy or other conditions.
Instrumental test
Patients should take an instrumental test, ultrasound 7.5–10 Mhz, which distinguishes the different components in the skin and the adipose tissue, such as water, fibrosis, and micro and macro nodules1. Measurements should include dermal thickness between the epidermal hyperechogenic line and the deep dermal line, and adipose tissue thickness between the dermal hyperechogenic line and the hyperechogenic muscular fascia.
Studies have proven that this examination not only shows the differences between localised adiposity and lipodystrophic panniculopathy, but also identifies the disease stage and provides control12,13. Therefore, it is an apt procedure to select the best therapeutic strategy and, above all, it helps the physician make a prognosis. It is performed with a 7.5 or 8 MHz transducer. A 20 MHz Scan C may be used for a more detailed study of the skin surface.
Videocapillaroscopy
The optical probe videocapillaroscope magnifies samples 10 to 1000 times, but a 200 magnification is normally used14. The videocapillaroscope works with an optical probe with epiluminescence and polarised light relayed to an image digitalisation system. It is a scientific research method used for angio-tectonic mapping, for studying microvessel responses to physical-mechanical and haemodynamic stimuli, as well as endocrine responses, and for monitoring drug therapies. For aesthetic pathologies, it represents the basic examination tool for skin, for the diagnosis of localised adiposities and lipodystrophy, and also for monitoring therapeutic responses.
The patient should remain in position in a neutral thermal environment and should not have smoked for the past 2 hours. Once the optical fibre or scope is in contact with the skin, different morphological aspects of regional microcirculation may be studied, in particular the regional angio-tectonic structure. Thus, blood microflow and aggregation or capillary alteration phenomena may be efficiently examined1.
The instrumental help of the videocapillaroscopy optical probe (VCOP), permits a clinical diagnostic classification that corresponds to histomorphological alterations and anatomotopography of the adipose tissue.
The VCOP is a noninvasive method that analyses capillaries in a static and dynamic form and when integrated with the digital images, transforms the qualitative to quantitative characteristics allowing comparative images taken at different times as well as comparisons of sequential images over time1.
Aesthetic pathology
Cellulite is an aesthetic pathological condition and treatments. should range from a review of lifestyle habits and behaviours to shaping surgery. This article will give an overview of the following:
- Nutritional endocrinology
- Skin care
- Body building-aerobic exercise
- Hormonal rebalancing
- Manual lymphatic drainage
- Platelet-rich plasma (PRP)
- Mesotherapy
- Carboxytherapy
- Endermologie
- Radiofrequency
- Liposculpture.
First steps
The objectives of cellulite treatment should be to:
- Restore local microcirculation
- Favour local metabolic exchanges
- Increase local proteoglycan-levels
- Increase veno-lymphatic drainage
- Increase lipolytic action (physiology lipolysis)
- Diminish fibrous trapping of adipocytes.
- The first step in the treatment should be the stimulation of microcirculation and the removal of accumulated fluids and toxic elements. This can:
- Improve the interstitial matrix basal regulation, (ECM regulation)
- Improve fibroblast activity
- Decrease interstitial oedema
- Increase lipolysis (physiology lipolysis — the reduction of the size of the fat cells with the release of glycerol and NEFA. The number of fat cells remain the same)
- Improve better oxygen and nutrition of the adipose tissue.
Treatment
Nutritional Endocrinology
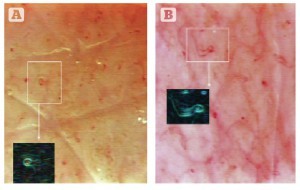
Figure 2 Treatment results viewed using the videocapillaroscopy optical probe. (A) Lack of microcirculation in the ischaemic area pre-treatment. (B) Post-treatment, observable microcirculation.
Food as a medicine has been referred to as pharmacy-nutrition or nutritional endocrinology15. In the efficacious nutritional therapy of cellulite, it has three targets15:
- Correcting overweight and obesity if present
- Increasing the blood flow
- Reducing inflammation.
Nutritional treatment of cellulite is not just a hypocaloric approach but is aimed at improving the state of tissue trophism and, in particular, at preventing and in some cases reducing the tissue phlogosis characteristic of the disease. With nutritional endocrinology, it relates to the stimulation using macro nutrients (carbohydrates, fats, and proteins) of specific hormonal systems (insulin-glycogen-eicosanoids), which may favour or damage the state of health in general and, in the case of cellulite, the worsening of the state of the tissues involved (adipose, connective, interstitial) in the glutei-femoral areas or on the inside of the knee.
The correction of overweight and/or obesity, may be reached by means of a reduction of the calorie intake, especially if derived from carbohydrates with a high glycemic index, which raise blood sugar levels with a consequent increase in levels of insulin.
Increasing the blood flow and reducing inflammation may be reached by means of a balanced diet of carbohydrates, proteins, and fats and is rich in fruit and vegetables, lean meat, fish, and mono-unsaturated fat such as olive oil. It is not only important to choose healthy foods but also to avoid substances contained in foods such as hydrogenated fats, interesterified oils, monosodium glutamate, and aspartame. It is also fundamental to propose nutritional models that are valid for a lifetime and not just for brief periods, so that the yo‑yo effect is avoided, which would cause a worsening of the initial state of the cellulite. The use of integrators, such as omega-3, vitamins, and minerals, must be evaluated to reduce the inflammation further15.
Food intolerance
Patients often have complex manifestations that involve all body systems. It is not unusual for a patient to present unique symptoms as articular pain, abdominal pain, reflux disease (GERD), colitis, cough, asthma, and skin allergies appearing after eating a particular food15. Most doctors are often unprepared to handle these type of phenomenon.
Overweight, obesity, and cellulite (even in underweight patients or those with alimentary behaviour disorders) can often be a side–effect of inflammation determined by food intake. This inflammation is both the concause and the main cause of all reactions related to lipodystrophy (cellulite). It may depend on a mean allergic reaction or from a hormonal imbalance in the adipokine production15,16,17.
Dietary supplementation
An important ‘cosmeceutic’ action led by dietary supplements helps the topical treatment of cellulite. It is important to remember, however, that ‘cellulite’ is a pathology, and thus the effects of both topical and systemic cosmeceutic treatments may only moderately relieve the typical appearance of cellulite: orange peel skin, lumps, pain in palpating, and colour of the complexion. Some examples include:
Bioflavonoids
Among the important substances used in ‘anti-cellulite’ supplements, bioflavonoids substantially help with microcirculation. The vegetal extracts mostly used are derivatives of ginkgo, black bilberry, grape, centella asiatica, pineapple, and melilotus. Substances contained in these vegetal extracts can protect capillaries, improve collagen and elastin synthesis, regulate platelet aggregation, and lower venous stagnation. The local oedematous situation should show an improvement of the peripheral circulation and the skin’s biomechanical proprieties18,19.
Hamamelis virginiana extra
The Hamamelis Virginiana (witch hazel) extract, used in a topical or systemic way, has an anti-inflammatory and protective action against the perivasal connective matrix degradation, which is the cause of the rising of capillary permeability and of chronic inflammation maintenance in phlebo-lymphatic stasis situations. Several studies20 have demonstrated that this extract can inhibit the action of some hormones like alpha-glucosidase, which are able to degrade the connective tissue.
Fatty acids
Omega-3 fatty acids are normally present in seafood, in certain plants and also in a number of animal products such as chicken, turkey, and eggs. Alpha-linolenic acid is the omega-3 fatty acid most extensively found in the vegetable world. This fatty acid has to be transformed into eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) in order to exercise the biological effects that are essential for the correct function of certain organs and elements (like the brain, retina, and gonads) and that protect against atherosclerosis and cardiovascular disease.
Glycine propionyl-L-carnitine
Dietary supplementation with the naturally occurring nutrient L-carnitine has been extensively studied as an aid to improve fatty acid metabolism and aerobic exercise capacity, to provide antioxidant benefits, and to enhance blood flow to active tissues.
While multiple forms of carnitine have been the focus of ongoing scientific study over several decades21, and several are currently available for retail sale, propionyl-L-carnitine (PLC) has been shown to provide optimal vasodilatory effect to blood vessels, and to support healthy heart and skeletal muscle function.
Those affected by cellulite can benefit from use of GPLC to help improve their pathological condition.
Body building aerobic exercise
Aerobic exercise is important for many reasons, one of which is because it allows the heart to release natriuretic peptides that have an important therapeutic action on the adipose tissue and other organs of the body.
Natriuretic peptides (NP) are a family of structurally similar endogenous peptide hormones that are mainly secreted by cardiomyocytes in response to a stress on the cardiac wall22. The metabolic roles of atrial NP (ANP) and B-type NP (BNP) were unsuspected until the discovery in 2000 that they exert potent lipolytic effects in human fat cells and increase plasma non-esterified fatty acid (NEFA) levels when infused intravenously22,23.
The induction of lipolysis and lipid mobilisation must be included in the numerous physiological actions of NPs. This induction is mediated by NPR-A, cGMP, and PKG. Studies22–24 have revealed the physiological relevance of this pathway during physical exercise in normal-weight young men, in obese men and women, and during head-down bed rest. An important source of energy during exercise is NEFAs originating from adipose tissue. In addition to catecholamines, ANP has an important role in the control of lipid mobilisation and NEFA availability in adipose tissue.
Hormonal rebalancing
Bioidentical hormone replacement therapy (BHRT) has been used in increasing numbers, particularly over the last 10 years, in many parts of the United States and Canada25–28. Subcutaneous pellet implants in men and women are gaining popularity due to convenience of application, dosing intervals, a low incidence of side‑effects and reported success among users. Testosterone therapy has been used to treat men and women of all ages diagnosed with testosterone deficiency. Subcutaneous oestrogen and testosterone therapy delivered by pellet implant has been used with success since 1938. BHRT uses hormones that are identical to the hormones manufactured by the body and has transformed the healthcare of men and women as they enter the second half of their lives.
Pellets or implants are made up of hormones (testosterone or oestrogen) that are pressed or fused into very small solid cylinders. These pellets are similar in size to a grain of rice. BHRT is often called ‘natural hormone therapy’ because the bioidentical hormones act just like the hormones produced by the body. With ageing, the body no longer produces adequate levels of oestrogen and testosterone, the hormones required to maintain the body. Subcutaneous pellets can replace the hormones that are lacking.
Pellets deliver consistent, healthy levels of hormones for 3–4 months in women and 4–5 months in men. Pellets have shown to be superior for relief of menopausal symptoms i.e. hot flushes and night sweats. Pellets do not increase the risk of blood clots, strokes or heart attacks unlike conventional or synthetic hormone replacement therapy. In studies, when compared to conventional hormone replacement therapy, oestrogen and testosterone pellets have been shown to increase bone density and muscle mass, restore sleep patterns and improve sex drive, sexual response, and overall well-being. Symptoms of low testosterone in women may include dysphoria (sadness, depression, anxiety and irritability), insomnia, decreased libido, hot flushes, decreased bone loss and muscle mass, and difficulty staying in shape.
Subcutaneous hormone treatment with pellets is a safe, effective, and convenient method of hormone delivery for symptoms of declining oestrogen and testosterone in women, and testosterone in men. Numerous studies in the literature25–28 have reported positive scientific evidence in regard to hormonal benefits, effectiveness, safety with minimal side‑effects and convenience of use and application. The delivery system and formulation has also proven superior when compared to synthetic compounds and other delivery systems.
Manual lymphatic drainage
Manual lymphatic drainage (MLD)29–30 is an essential complementary therapy for cellulite. It should be gentle and non-traumatic in order to provide improved tissue metabolic homeostasis. Manual lymphatic drainage follows Foldi’s and Leduc’s teachings. It consists in a series of gentle touches and compressions over specific lymphatic system sites aimed at emptying congested ganglia and improving lymphatic flow by removing lymph from tissues.
The rules of MLD:
- Stimulate the microcirculation to improve oedema and cellular nutrition
- Do not produce pain during the massage
- 30–40 minutes is needed to perform good MLD
- Do not produce skin redness during the MLD
- Do not use creams
- Only use the hands and the correct techniques to mobilise the lymph
- The aim is to move lymph and high protein from the interstitial into the small lymphatic vessels.
Remember, the softer the tissues, the lighter the pressure.
Platelet-rich plasma
Platelet-rich plasma (PRP) is an autologous high concentration of human platelets in a small volume of plasma measured as 1,000,000 platelets per mm3 or two to three times the native concentration of whole blood at a pH of 6.5–6.7 (whole blood pH is 7.0–7.2)31.
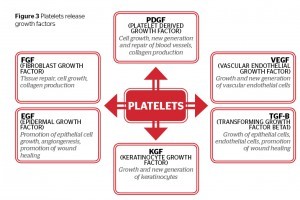
PRP is made up of the fundamental protein growth factors which have been proven to be actively secreted by platelets to initiate all wound healing31.
As PRP is a concentration of platelets, it is also a concentration of the seven fundamental protein growth factors proven to be actively secreted by platelets to initiate all wound healing. These growth factors include:
- The three isomers of platelet derived growth factors
- Two of the numerous transforming growth factors (TGF1 and TGF2)
- Vascular endothelial growth factor (VEGF) and epithelial growth factor (EGF).
All these growth factors have been documented to exist in platelets32,33.
The biologically active signal peptides released from local tissue or blood products (particularly the platelet fraction) play a critical role in influencing the initiation and progression of the normal wound healing process. Such factors coordinate the processes of epithelialisation, angiogenesis, and collagen-matrix formation, the key steps in the wound healing sequence.
Growth factors function in paracrine, endocrine, and autocrine manners in order to guide the dynamic stages of wound healing. No single growth factor appears to maintain a total physiologic task, but instead these peptides work in a coordinated fashion to orchestrate the normal wound healing processes.
Besides the initiation of coagulation processes, the platelets undergo a degranulation process which releases a complex group of growth factors and cytokines (peptides) essential for wound-healing mechanisms.
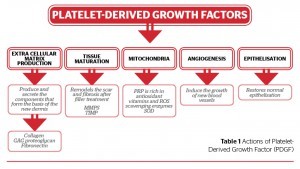
In Table 1, it is possible look at the different actions of the platelet-derived growth factor over the extracellular matrix and tissue maturation, against the free radicals, and in relation to angiogenesis and epithelisation.
PRP under the concentration of the growth factors gives a strong and autologous medicine for the fibroblast stimulation, helps the recovery of the ECM, increases the angiogenesis and helps the recovery of the skin with the production of collagen. This is a process of biostimulation and is the main motivation for the PRP. Biostimulation activates the biological functions of the skin with the purpose of optimising its physiology and consequently leading to aesthetic improvement. This is part of the author’s base treatment in all cases of cellulite.
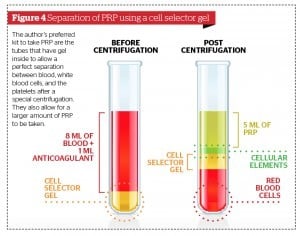
Obtaining PRP
There are many kits for obtaining PRP. In the author’s opinion the best kits have gel inside the tubes to allow a perfect separation between blood, white inflammatory cells, and plasma.
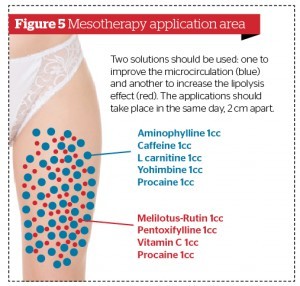
Mesotherapy
Mesotherapy consists of the introduction of drugs into the superficial subcutaneous skin34. The injections use minimal amounts of drugs as a complement to routine clinical procedures. The amount of the injection is determined by the proximity of the injection site to the site of the pathology34,35.
Five-stage treatment with mesotherapy
Mesotherapy, along with carboxytherapy and manual lymphatic drainage, is recommended by the author as the first step in treating cellulite. The author’s favoured protocol when using mesotherapy begins with biostimulation with PRP to help connective tissue recovery and microcirculation. The author then introduces different medications depending on the pathology of the individual patient using an automatic electronic mesogun. The five-stage treatment is as follows:
- Biostimulation PRP as discussed above
- Reduce lipoedema by using Melilotus plus pentoxifylline and procaine
- Restore efficient microcirculation by using:
- Derivatives of flavonoids, such as rutin or melilotus, which offer particularly beneficial vasculo-protective effects
- Vitamin C, which is essential for neutralising the effect of the free radicals generated in the newly-oxygenated tissue (reperfusion syndrome)
- Lipolysis using theophylline + carnitine + caffeine + yohimbine + procaine. This helps to:
- Inhibit phosphodiesterase
- Maintain a high level of cyclic activated protein kinase (AMP)
- Stimulate the natural lipolytic mechanisms of the adipocytes
- Restructuring and protecting the connective tissue by DMAE to stimulate the regeneration of connective tissue.
Carboxytherapy
Carboxytherapy refers to the therapeutic use of carbon dioxide (CO2) in its gaseous state, either transcutaneous or by subcutaneous injection.
At the vascular level, CO2 increases vascular tone and produces active microcirculatory vasodilatation due to its direct activity on arteriole smooth muscle cells.
In addition, this promotes the Bohr effect, a mechanism that allows tissue CO2 to transfer to the lungs and oxygen present in the lungs to transfer to tissues through the oxyhaemoglobin dissociation curve. When administered through an external route, CO2 promotes this mechanism, resulting in a higher tissue oxygenation and neoangiogenesis.
The effects of C02 are to36–38:
- Increase tissue oxygenation
- Increase flow rate and vasodilatation
- Clean the ECM
- Improve the lipolytic effect due to an increase in oxidative process.
Clinical Results
The increase of microcirculation improves the metabolism in the connective tissue and help to recover the health of the extracellular matrix. The following are the clinical results:
- Slight loss of local adiposity
- Big improvement to the appearance of the skin so that it appears more compact and elastic
- Decrease in the dimple effect. The CO2 reverts this situation when injected in the affected zones through a very thin needle as it:
- Produces vasodilatation
- Improves the speed of the microcirculation
- Ensures the tissue receives more oxygen so the toxins are eliminated
- Reduces the oedema
- Favours the lipolysis.
Carboxytherapy also provides excellent results for patients with long-time cellulite, and young patients as a prevention method.
Endermologie
Enermologie is a particularly effective treatment in the activation of fibroblasts and the metabolism of the interstitial matrix. It represents a more important basic treatment for different forms of cellulite.
Endermologie acts on the skin and subcutaneous tissue, connective tissue, fat tissue, and the microcirculation both arteriolar, venous and lymphatic and has shown beneficial effects on:39–41
- Venous and lymphatic circulation
- Skin trophicity
- Fibrosis
- Adipose tissue (increase the physiology lipolysis).
Radiofrequency
The proposed mechanisms for efficacy of radiofrequency in cellulite treatment include thermal injury leading to tightening of dermal fibrous septae, formation of new collagen and collagen remodelling. This should improve the skin’s firmness and elasticity. Please note that radiofrequency increases the formation of fibrosis and this is not a physiological process.
Liposculpture
A liposculture is a technique for fat tissue extirpation through blunt 2–4 mm cannula, and suction may be carried out with 20 or 60 cc syringes or a suction pump. It aims to remodel contours to restore the juvenile and harmonic forms of the face or body by working with the hypodermic fatty tissues42.
Laserlipolysis
Laserlipolysis is an advanced technique for the removal of localised excess of fatty tissue that can be used alongside or in combination with traditional liposuction to improve results.
The technique uses the high peak power of the laser emission to rupture the membrane of the adipocytes. The effect is not only thermal but also thermomechanical, and the rapid and elevated absorption by the adipocyte membrane allows for creating an opening in the membrane itself with the spilling out of the cellular contents. The mix of the cell contents and the fluids from the tumescent anaesthesia result in the production of an oily, low-viscosity aggregate which facilitates body modelling, and can be easily removed with low-pressure micro-pumps. The author suggests removing the emulsion with a 2 mm cannula and a 20 cc syringe.
The first device was a Nd:YAG laser, at a 1064 nm wave-length, using 6 W power, 40 Hz frequency, 150 mJ energy, and 100 ms pulse. Today we have 10 W, 18 W, and 30 W devices43,44.
There are new Laserlipolysis devices that work with two different wavelengths and claim to treat cellulite in just one session. These lasers only release the fibrotic retraction of the connective tissue; they do not alter the ECM.
Whilst it is important to share experiences with other colleagues at meetings it is essential to practice the skills that any surgical techniques require to maximise patient safety and results. Technological advances in surgical procedures continue apace and physicians should have up-to-date knowledge and skills prior to incorporating any new techniques to their practices.
As President of the International Union of Lipoplasty, the author is keen to promote, support, and encourage the learning process in this area to ensure patient safety and raise the standards across the industry.
Protocols
To improve the results of cellulite treatments it is useful to combine different techniques and so benefit from the different actions/effects.
Steps in the treatment
Step 1: Keep the connective tissues elastic and soft. Improve the ECM
- PRP
- Endermologie
- Carboxytherapy
- MLD
Step 2: Improve the microcirculation
- Carboxytherapy
- Endermologie
- Mesotherapy
Step 3: Action to increase fibroblast activity
- Endermologie
- Mesotherapy
- Carboxytherapy
- PRP
Step 4: Action to tighten the skin
- Radiofrequency
- Carboxytherapy
- Mesotherapy
Step 5: Anti-inflammatory action
- Endermologie
Step 6: Anti-fibrotic action
- Endermologie
Step 7: Reduction of the fat tissue
Non-surgical
- Mesotherapy
- Carboxytherapy
- Endermologie Cryolipolysis (there are doubts about the physiology action)
- HIFU (there are doubts about the physiology action)
Surgical
- Lipoplasty
- Laserlipolysis.
Conclusions
Today, the pathophysiology of cellulite is well known and there is a good body of research on the subject. It is impossible to say that a single method or medical device can treat it and there are many variables that must be taken into account to achieve a good medical aesthetic results for patients.
In summary, the author recommends the following treatment scheme:
- Restore local microcirculation
- Favour local metabolic exchanges
- Reduce the oedema
- Clean the ECM
- Increase local proteoglycan-level
- Increase venolymphatic drainage
- Increase lipolytic action (physiology action over fat tissue)
- Diminish fibrous trapping of adipocytes.